Isoniazid Hepatotoxicity: What You Need to Know About Liver Risks from TB Medication
When you take isoniazid, a first-line antibiotic used to treat tuberculosis. Also known as INH, it’s one of the most effective drugs for stopping TB—but it can also damage your liver in ways that aren’t always obvious. This isn’t rare. About 1 in 10 people on isoniazid develop mild liver enzyme changes, and up to 1 in 250 may get serious liver injury. Most cases show up within the first 2 to 3 months of treatment. The risk goes up if you’re over 35, drink alcohol regularly, have hepatitis B or C, or are taking other meds that affect the liver.
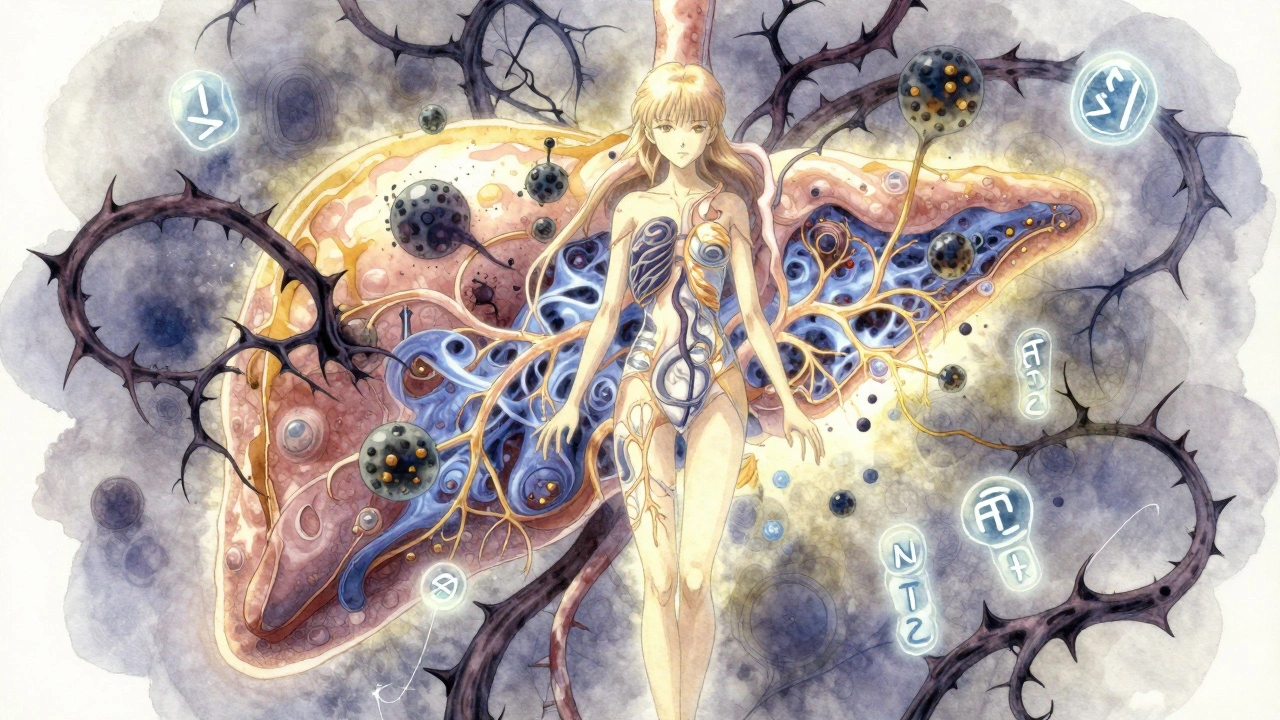
What makes isoniazid hepatotoxicity, a type of drug-induced liver injury caused by the body’s reaction to isoniazid tricky is that it often doesn’t cause symptoms at first. No nausea, no yellow skin—just a silent rise in liver enzymes on a blood test. That’s why regular monitoring is critical. Doctors check ALT and AST levels before you start and then every 4 to 8 weeks. If levels jump more than 3 times the upper limit of normal—or if you start feeling unusually tired, dark urine, or right-side belly pain—you stop the drug immediately. It’s not a guess. It’s a protocol backed by decades of clinical data.
The good news? Most people never have a problem. And if you do, stopping isoniazid usually lets your liver recover fully. But here’s what matters: not everyone gets the same risk. Older adults, women, and people with HIV or malnutrition are more vulnerable. Some genetic variations also make your liver process the drug differently, increasing toxicity. That’s why some clinics now test for specific gene markers before prescribing it. You don’t need a fancy test to stay safe—you just need to know the signs and show up for your blood work.
It’s not just about isoniazid. It’s about how it fits with other things you take. alcohol, a known liver stressor that multiplies the risk of isoniazid damage should be avoided completely during treatment. Same with acetaminophen, a common pain reliever that adds strain to an already stressed liver. Even herbal supplements like kava or green tea extract can push things over the edge. Your pharmacist should flag these interactions—but you need to speak up too.
What you’ll find below are real, practical guides from people who’ve lived through this. From how to track your symptoms at home, to what labs to ask for, to how to talk to your doctor when you’re worried. No fluff. No jargon. Just what works when your liver is on the line.