Autoimmune hepatitis isn’t something you catch from someone else. It’s not caused by alcohol, viruses, or poor diet. It’s your own immune system turning against your liver. Think of it like a friendly fire incident inside your body - the soldiers meant to protect you start attacking your liver cells instead. This leads to ongoing inflammation, scarring, and if left untreated, cirrhosis or liver failure. The good news? We know how to stop it. And the backbone of that treatment has been the same for over 50 years: steroids and azathioprine.
How Do Doctors Know It’s Autoimmune Hepatitis?
There’s no single blood test that says, "Yes, this is autoimmune hepatitis." That’s why diagnosis is a puzzle. Doctors piece together clues from blood work, imaging, and a liver biopsy.
First, they check liver enzymes - ALT and AST. In active autoimmune hepatitis, these are often 5 to 10 times higher than normal. Then they look at IgG, a type of antibody. If it’s more than 1.5 times the upper limit of normal, that’s a red flag. Autoantibodies like ANA (antinuclear antibodies) or SMA (smooth muscle antibodies) are also common. About 80% of cases show these markers. A less common type, called type 2 AIH, has LKM1 antibodies, but it’s rare and doesn’t change how you’re treated.
Here’s the key: you have to rule out everything else. Viral hepatitis (A, B, C), alcohol-related damage, fatty liver disease, drug reactions - all of these can mimic autoimmune hepatitis. Blood tests for hepatitis B and C are mandatory before starting treatment. Why? Because if you have a hidden hepatitis B infection and start immunosuppressants, it can flare up dangerously.
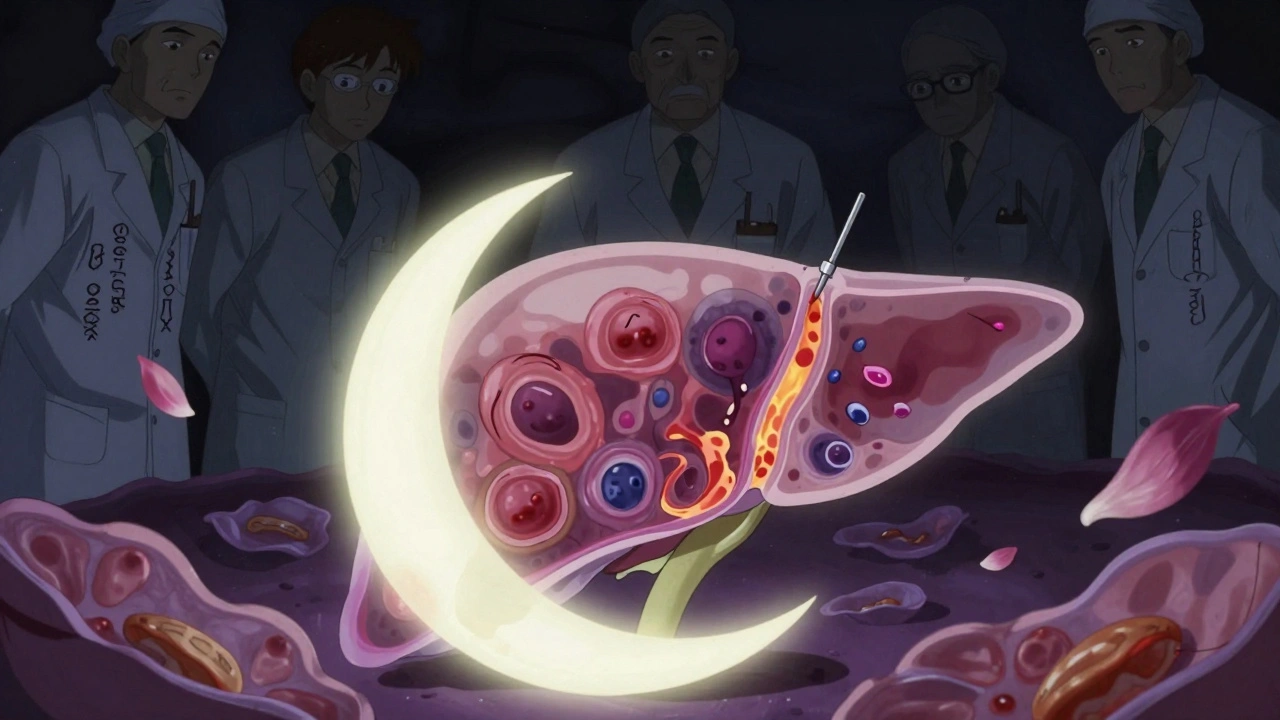
The real gold standard is the liver biopsy. A small sample of liver tissue is taken using a thin needle guided by ultrasound. It’s low-risk - serious complications happen in less than 0.3% of cases. Under the microscope, pathologists look for something called interface hepatitis: inflammation right where the liver’s portal areas meet the healthy tissue. If this pattern shows up in at least 20 portal tracts, it’s almost certainly autoimmune hepatitis.
Doctors use a scoring system called the Revised IAIHG criteria. Points are added for symptoms, blood markers, biopsy findings, and excluding other causes. A score over 15 means probable AIH. Over 20? Definite AIH. No more guessing.
Why Steroids Are the First Line of Defense
Since the 1970s, corticosteroids like prednisone or prednisolone have been the go-to treatment. They work fast. In fact, 80 to 90% of patients show improved liver enzyme levels within two weeks. That’s not just a statistic - it’s a lifeline.
The typical starting dose is 0.5 to 1 mg per kilogram of body weight per day - up to 60 mg daily. For someone weighing 70 kg, that’s about 35 to 70 mg. It’s not a small amount. But it’s necessary to shut down the immune attack quickly.
Here’s the catch: steroids come with a heavy side effect list. Moon face. Weight gain. Mood swings. Insomnia. High blood sugar. Bone thinning. Cataracts. About 70% of people on steroid-only treatment develop at least one major side effect within five years. One patient on Reddit described it as "moon face that made me unrecognizable, 30 pounds of fluid weight in three weeks, and insomnia that felt like permanent jet lag."
That’s why steroids aren’t meant to be taken long-term alone. They’re the sledgehammer. The goal is to use them to get the disease under control, then get you off them as fast as safely possible.
Azathioprine: The Steroid-Sparing Partner
Azathioprine - sold under brand names like Imuran or as a generic - is the quiet hero in this story. It doesn’t work fast. It takes weeks to months to kick in. But it’s the reason you can survive long-term treatment.
Azathioprine is an immunosuppressant. It doesn’t kill immune cells - it slows them down. When combined with steroids, it allows doctors to cut the steroid dose by 70 to 80% within six months. That cuts side effects in half. Instead of 70% of patients suffering from steroid damage, it drops to 30%.
The starting dose is usually 50 mg per day, slowly increased to 1 to 2 mg per kg per day - up to 150 mg. It’s taken daily, often for years.
But azathioprine isn’t risk-free. About 35% of people get stomach issues - nausea, vomiting, diarrhea. Around 12% experience bone marrow suppression, which can drop white blood cell counts dangerously low. That’s why testing for TPMT enzyme levels is now standard before starting. TPMT is a liver enzyme that breaks down azathioprine. If you have a genetic variant that makes you TPMT-deficient (about 0.3% of people), even a normal dose can cause life-threatening toxicity. Testing costs $250-$400 in the U.S., and 89% of academic centers now do it routinely.
One patient shared on the American Liver Foundation forum: "Azathioprine caused pancreatitis at 100 mg. I had to switch to mycophenolate after 18 months of trial and error." That’s the reality - not everyone tolerates it. But for most, it’s the difference between living with side effects and living with a failing liver.
How Long Do You Take This Treatment?
There’s no fixed timeline. Some people feel better in months. Others take years.
Complete biochemical response - meaning ALT, AST, and IgG levels return to normal - happens in 60 to 80% of patients within 18 to 24 months. But that doesn’t mean you’re cured. It means the disease is controlled.
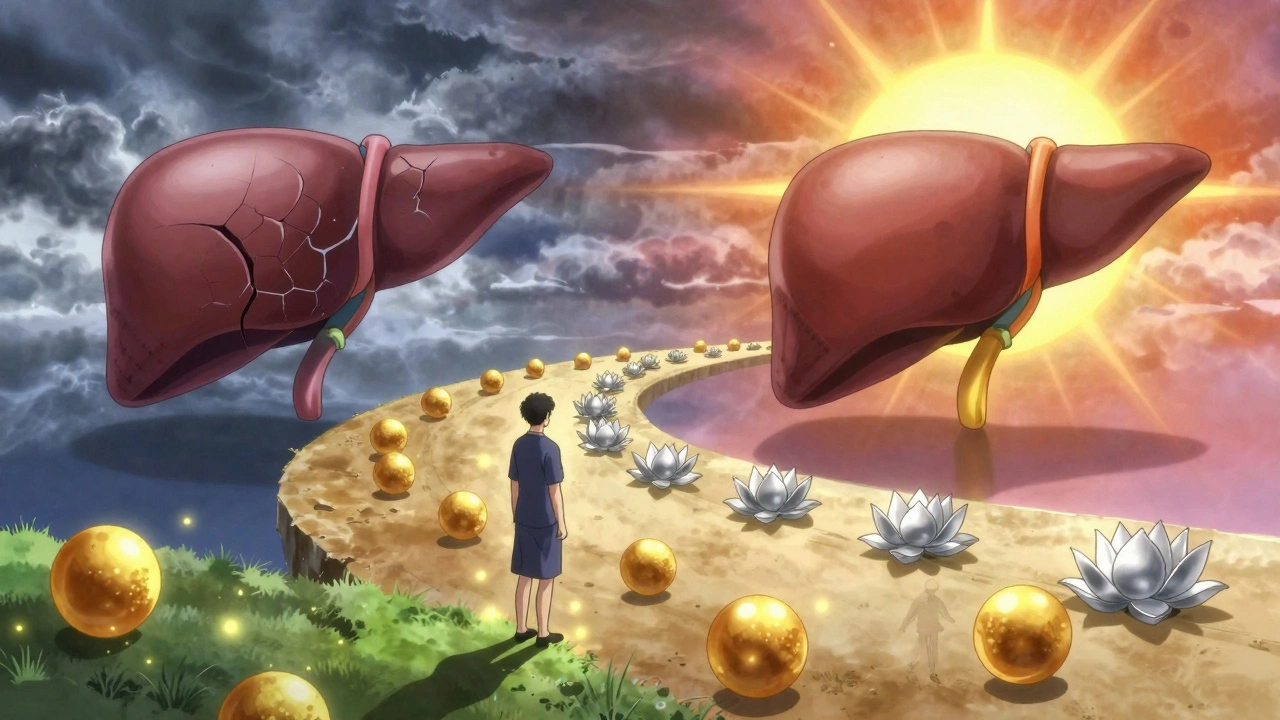
Doctors recommend a second liver biopsy after 2 to 3 years of treatment to check for histological remission - meaning the inflammation and scarring have actually reversed. Studies show 50 to 70% of patients achieve this. That’s huge. It means your liver can heal.
Here’s the hard truth: 60 to 80% of patients need lifelong maintenance therapy. Why? Because stopping treatment too soon leads to relapse in 50 to 90% of cases. Even if you feel fine, your liver might still be quietly inflamed.
Some patients do try to stop. The 2025 EASL guidelines say it’s okay - but only if you’ve had at least 2 years of complete remission, and you taper slowly over 6 to 12 months. Even then, 70% of relapses happen within three months of stopping. That’s why monitoring continues for life - liver tests every 3 months, even if you’re stable.
What If Steroids and Azathioprine Don’t Work?
Most people respond. But 10 to 15% don’t. That’s called treatment failure. Or maybe you can’t tolerate the side effects. That’s treatment intolerance.
When that happens, doctors turn to second-line drugs. Mycophenolate mofetil (CellCept) is the most common. It’s taken twice daily and tends to be easier on the stomach than azathioprine. It’s also less likely to cause bone marrow suppression. About 60% of patients who switch to mycophenolate see improvement.
Other options include calcineurin inhibitors like tacrolimus or cyclosporine. These are powerful and require careful blood level monitoring. They’re used when other drugs fail.
And there’s new hope on the horizon. The FDA gave obeticholic acid (Ocaliva) breakthrough therapy status in 2024 for AIH. In early trials, it showed a 42% complete response rate - better than the 28% with standard therapy. JAK inhibitors like tofacitinib and monoclonal antibodies targeting interleukin-6 are also in phase 2 trials. These aren’t available yet, but they’re coming.
What You Need to Do Before and During Treatment
Before starting steroids or azathioprine, you need a few things in place:
- Get tested for hepatitis B - if positive, you’ll need antiviral protection.
- Get vaccinated for hepatitis A and B - vaccines work poorly once you’re immunosuppressed.
- Have a TPMT test done - it’s non-negotiable before azathioprine.
- Get a bone density scan - steroids weaken bones. You may need calcium, vitamin D, or bisphosphonates.
- Start monitoring your blood sugar - steroids can trigger diabetes.
During treatment:
- Check liver enzymes every 2-4 weeks at first, then every 3 months.
- Get IgG levels checked quarterly.
- See your doctor if you get a fever, sore throat, or feel unusually tired - it could be low white blood cells.
- Take your meds at the same time every day. Missing doses increases relapse risk.
- Don’t drink alcohol. Ever.
And remember: this isn’t a sprint. It’s a marathon. The goal isn’t just to feel better. It’s to protect your liver for decades.
Real People, Real Results
Not everyone’s story is the same. One woman on HealthUnlocked wrote: "After 2 years on 5 mg prednisone + 75 mg azathioprine, my biopsy showed complete fibrosis reversal from F3 to F0." That’s not just hope - that’s science. The liver can regenerate. Even after scarring, treatment can undo damage.
Another patient said: "The side effects were worse than the disease." That’s true for many. But without treatment, the disease wins. With it, most people live full, normal lives. The 2025 EASL guidelines say the 10-year survival rate for treated AIH is over 90% - nearly the same as the general population.
The key is sticking with it. Even when it’s hard. Even when you feel fine. Even when the pills make you feel like a stranger in the mirror. Your liver is fighting for you. You just have to help it win.



John Filby
December 1, 2025 AT 21:29Man, I remember when I first got diagnosed. Thought I was just tired from work. Turns out my liver was screaming. Steroids made me look like a balloon animal, but hey - at least I’m still here.
Carolyn Ford
December 3, 2025 AT 13:31Wow. So you're telling me we're just throwing steroids at people like it's 1987? No wonder so many end up with diabetes and osteoporosis. This is medical malpractice disguised as protocol.
George Graham
December 5, 2025 AT 04:19I get what you're saying, Carolyn - but the alternative is liver failure. I’ve seen it. My cousin didn’t take the meds because he thought it was "too harsh." He needed a transplant by 38. Sometimes the side effects are the price of staying alive.
Yasmine Hajar
December 5, 2025 AT 23:30TO ALL THE PEOPLE WHO THINK THIS IS JUST "TAKING PILLS" - IT’S NOT. It’s waking up with moon face, crying because you don’t recognize yourself, then swallowing a pill anyway because you know your liver is counting on you. You’re not weak for struggling. You’re brave for continuing.
Gillian Watson
December 6, 2025 AT 19:24My mate in Manchester got diagnosed last year. Started on prednisone - lost 15kg of muscle in 3 weeks. Then switched to mycophenolate. Now he’s hiking in the Lakes. Took 18 months. But he’s alive. And that’s the win.
Ben Choy
December 8, 2025 AT 06:27TPMT testing is non-negotiable. Seriously. My cousin died from azathioprine toxicity because they skipped it. $300 saved his life. Why isn’t this mandatory everywhere?
Shofner Lehto
December 8, 2025 AT 12:21Just want to say thank you for writing this with such clarity. I’m a nurse and I’ve seen too many patients get scared off by side effects. This is the kind of info that saves lives - not just stats, but real human context.
Martyn Stuart
December 9, 2025 AT 23:19One thing missing: the psychological toll. You’re not just managing a liver - you’re managing the fear that every headache is a flare, every fatigue is a relapse. The mental load is heavier than the pill bottle.
Alex Piddington
December 10, 2025 AT 02:25Great breakdown. I’d add that many patients don’t realize that fibrosis reversal is possible. I’ve seen F3 → F0. It’s not magic - it’s science. And it’s why we don’t give up.
Elizabeth Crutchfield
December 10, 2025 AT 18:28i had the azathioprine nausea for like 3 months… then it just… stopped. like magic. but i was so scared to keep taking it. like what if i die? what if i dont? what if my liver hates me? idk.
Jordan Wall
December 12, 2025 AT 00:44It’s fascinating how we still rely on 1970s pharmacology for such a complex immunological disorder. The fact that we haven’t moved to targeted biologics as first-line is a systemic failure. Ocaliva’s 42% response rate? That’s the future. Why are we still playing whack-a-mole with steroids?
Emmanuel Peter
December 13, 2025 AT 22:37Everyone’s so nice about this, but let’s be real - this treatment is torture. You’re not "surviving," you’re existing. And the fact that 80% need lifelong meds? That’s not a win. That’s a life sentence.
Ashley Elliott
December 15, 2025 AT 13:49Chad - I hear you. And I’ve been there. But here’s the thing: my biopsy last year showed no inflammation. My liver healed. I’m not "surviving." I’m living. It took years. But it happened. Don’t give up on the process.
Chad Handy
December 17, 2025 AT 12:09Let me tell you about the 47-year-old woman I saw last month. She was on steroids for 11 years. Moon face, cataracts, diabetes. She cried every time she took her pill. But she never missed one. Last week, her biopsy showed fibrosis reversal. She’s now on 5mg azathioprine. She’s not cured. But she’s alive. And she’s proud. That’s not a failure. That’s a victory.
People think medicine is about quick fixes. It’s not. It’s about showing up, every damn day, even when you hate yourself for needing it.
And yeah - the side effects suck. But the alternative? You don’t get to see your kid graduate. You don’t get to hold your grandbaby. You don’t get to watch the sun rise on another Tuesday.
So yeah. Take the pill. Even if you hate it. Even if you hate yourself for needing it. Your liver doesn’t care why you’re taking it. It just cares that you did.
And that’s enough.
Chase Brittingham
December 18, 2025 AT 14:07I’ve been on azathioprine for 7 years. No moon face. No diabetes. Just a little nausea sometimes. My TPMT was normal. My liver enzymes are perfect. I still get scared every time I miss a dose. But I take it. Because I owe it to the version of me that didn’t know this was coming.
Jake Deeds
December 19, 2025 AT 16:11Look, I get it. You’re all being so noble about the pills. But let’s be honest - this whole system is designed to keep you dependent. Pharma loves lifelong meds. And doctors? They’re not trained to say "you might be able to stop." They’re trained to say "stay on it."
My doctor told me I’d be on this forever. I asked for a trial off. He said no. So I did it anyway. Tapered slowly. 18 months later - zero relapse. My IgG is normal. My biopsy is clean.
Maybe you’re one of the 20% who can stop. Maybe you’re not. But don’t let fear make the decision for you.
Rudy Van den Boogaert
December 20, 2025 AT 13:21Just had my 3-year biopsy. F0. No fibrosis. No inflammation. I’ve been on 5mg prednisone + 75mg azathioprine since day one. I still get tired. I still get anxious. But I’m here. And I’m not just surviving - I’m teaching piano to kids, hiking with my wife, laughing at stupid memes. This isn’t a cure. But it’s a life. And that’s worth every pill.
michael booth
December 22, 2025 AT 08:37Thank you for this comprehensive, evidence-based overview. The inclusion of real patient narratives elevates this from clinical text to human experience. It is imperative that healthcare providers recognize that adherence is not merely a matter of compliance - it is an act of profound self-advocacy in the face of systemic indifference. Continued research into targeted immunomodulators remains paramount.