LDAA Dosing Calculator
Metabolite Assessment Tool
This tool determines if a patient is suitable for low-dose azathioprine and allopurinol (LDAA) therapy based on therapeutic metabolite levels.
Enter metabolite levels to see assessment
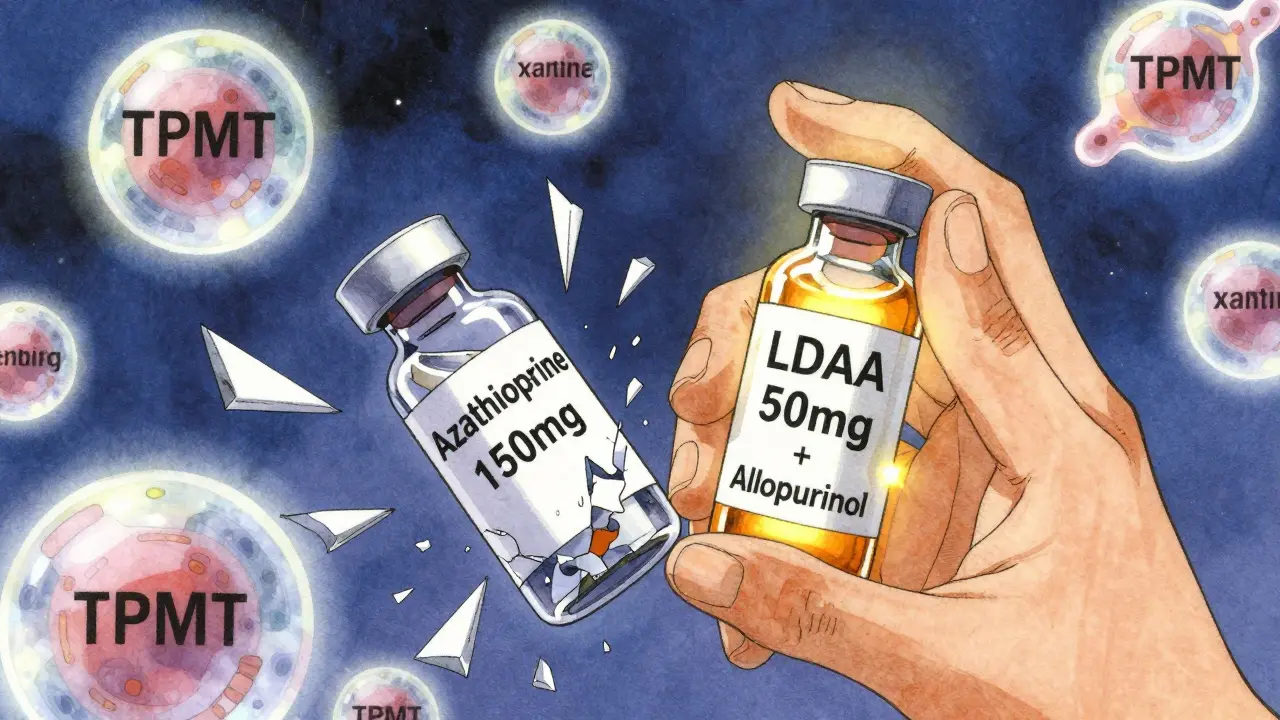
When azathioprine doesn’t work-or makes you sicker-doctors have a secret weapon: low-dose azathioprine with allopurinol, or LDAA. It’s not a new drug. It’s a smarter way to use two old ones. For patients with inflammatory bowel disease (IBD) or autoimmune hepatitis who can’t tolerate standard azathioprine, this combo flips the script. Instead of letting toxic metabolites build up and wreck the liver, it redirects the body’s metabolism to boost healing and shut down harm. But get it wrong, and you risk life-threatening bone marrow suppression. This isn’t guesswork. It’s precision medicine, grounded in hard science and strict protocols.
Why Azathioprine Alone Can Backfire
Azathioprine has been used since the 1960s to calm overactive immune systems. It’s cheap, effective for many, and often the first choice for IBD patients who don’t respond to steroids. But for 15-20% of people, something goes wrong. Their bodies convert too much of the drug into 6-methylmercaptopurine (6-MMP), a metabolite that doesn’t help the immune system-it just damages the liver. These patients are called "hypermethylators." They have high levels of an enzyme called TPMT, which shunts azathioprine down the wrong path. Their 6-TGN levels (the good metabolite that suppresses inflammation) stay low, while their liver enzymes climb. Many are told to stop azathioprine entirely. But there’s another option.The Allopurinol Trick: Redirecting Metabolism
Allopurinol was designed for gout. It blocks xanthine oxidase, an enzyme that breaks down uric acid. But in the 1990s, researchers noticed it also blocks another enzyme involved in azathioprine metabolism. That’s when the idea clicked: if you shut down the pathway that makes 6-MMP, the drug gets pushed toward the therapeutic 6-TGN pathway instead. It’s like closing a leaky faucet so water flows where it’s supposed to. When you give allopurinol (100 mg daily) with a drastically reduced dose of azathioprine (50 mg instead of 150-200 mg), 6-MMP drops by 70-90%. At the same time, 6-TGN rises 2-5 times. The result? Liver enzymes normalize. Inflammation drops. Patients get back to normal life.How It Works: The Metabolic Switch
Azathioprine breaks down into 6-mercaptopurine (6-MP). From there, three things can happen:- Pathway 1 (Good): 6-MP turns into 6-thioguanine nucleotides (6-TGN) via HGPRT. These get into DNA and calm immune cells. Therapeutic range: 230-450 pmol/8×10⁸ RBCs.
- Pathway 2 (Bad): 6-MP becomes 6-MMP via TPMT. This causes liver damage. Safe level: under 2,800 pmol/8×10⁸ RBCs.
- Pathway 3 (Wasted): 6-MP turns into 6-thiouric acid via xanthine oxidase. This is inactive. No benefit.
Allopurinol shuts down Pathway 3. That forces more 6-MP into Pathway 1. But here’s the catch: if you don’t lower the azathioprine dose, you overload Pathway 1. That’s when 6-TGN spikes past 450 pmol/8×10⁸ RBCs-and your bone marrow starts shutting down. White blood cells crash. Neutrophils vanish. You get fevers, infections, hospital stays. That’s why LDAA isn’t just combining two drugs. It’s a delicate balancing act.
Who Benefits Most-and Who Should Avoid It
LDAA works best for patients with:- High 6-MMP (>5,700 pmol/8×10⁸ RBCs)
- Low 6-TGN (<230 pmol/8×10⁸ RBCs)
- Elevated liver enzymes (ALT/AST) on standard azathioprine
- TPMT activity above 14.2 U/mL (intermediate or high)
It fails for people with:
- TPMT deficiency (<5 U/mL)-they’re already at high risk for bone marrow failure
- Severe kidney disease (creatinine clearance under 30 mL/min)
- Pre-existing low white blood cell count
Studies show 65-75% of hypermethylators achieve remission on LDAA. Compare that to 30-40% on regular azathioprine. And in 85-90% of cases, liver damage reverses. But if you skip the dose reduction? You’re gambling with your life.
The Monitoring Protocol: No Exceptions
This isn’t a "take it and see" situation. Every patient on LDAA needs a strict monitoring plan:- Baseline: TPMT test, complete blood count (CBC), liver enzymes, 6-TGN and 6-MMP levels.
- Start: Azathioprine at 50 mg/day. Allopurinol at 100 mg/day.
- Weeks 1-4: CBC every week. Liver enzymes every 2 weeks.
- Week 4: Repeat 6-TGN and 6-MMP levels. Target: 6-TGN between 230-450, 6-MMP under 2,800.
- After Week 4: CBC every 2 weeks for 3 months, then monthly.
Delayed neutropenia is real. About 15-20% of patients hit a low white count between weeks 4 and 8. Most bounce back if you pause azathioprine for a week and restart at 25 mg. Permanent stoppage? Only if levels stay dangerous after adjustment.
Real Stories: Success and Scare
On patient forums, the stories split down the middle. One user, u/CrohnsWarrior2020, wrote: "After 3 years of failed treatments and sky-high liver enzymes, LDAA fixed everything. My liver is normal. I’m in remission. No side effects." That’s the dream. But another, u/UlcerativeColitisNewbie, shared: "I started LDAA without monitoring. My neutrophils dropped to 0.8. I ended up in the hospital with a fever. Now I’m terrified of all meds." That’s the nightmare. Both cases had the same drugs. Only one had the protocol.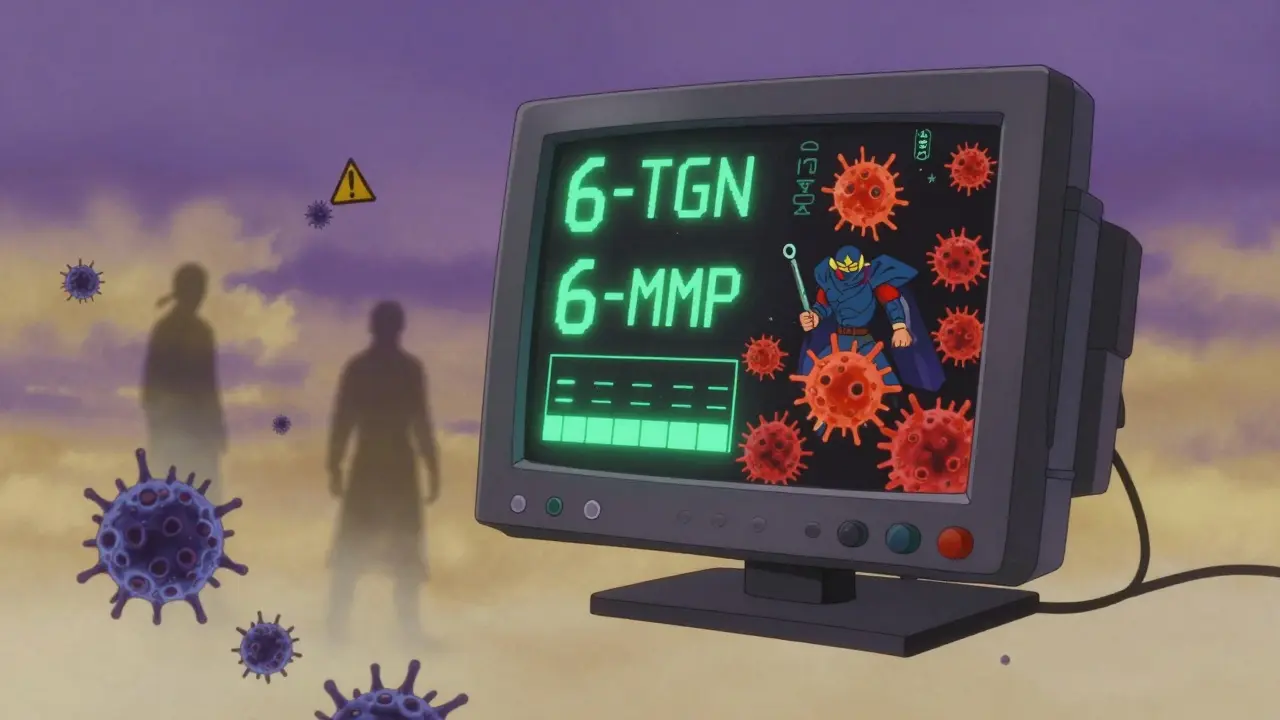
Why Doctors Are Still Hesitant
Some clinicians avoid LDAA because of a 1981 FDA warning about fatal bone marrow suppression. That warning came from cases where patients got full-dose azathioprine with allopurinol-no dose reduction. Today’s guidelines are clear: 25-33% azathioprine dose. The risk isn’t the combo. It’s the mistake. European guidelines from ECCO and AGA now endorse LDAA as a second-line option. In 2022, 65% of European IBD centers used it routinely. In the U.S., adoption lags at 35% in community practice. Why? Fear. Lack of training. No access to metabolite testing. But in academic centers, where monitoring is standard, usage hits 78%.The Bigger Picture: Cost, Access, and Future
LDAA costs $1,200-$1,800 a year. A single biologic like Humira? $30,000-$50,000. For patients without good insurance, or in countries with limited healthcare budgets, LDAA is a game-changer. It’s not just effective-it’s equitable. The future is faster testing. Two companies are developing point-of-care devices to measure 6-TGN and 6-MMP in under 2 hours. Right now, you wait weeks for results. In 2027, your doctor might adjust your dose before you leave the clinic.What You Need to Do
If you’re on azathioprine and your liver enzymes are high-or you’re not getting better-ask your doctor about LDAA. But don’t just ask. Ask for:- TPMT testing
- Therapeutic drug monitoring (6-TGN and 6-MMP levels)
- A clear plan for weekly blood tests for the first month
Don’t accept a prescription without it. This isn’t risky because it’s new. It’s risky because it’s powerful-and power demands precision.



Joie Cregin
January 16, 2026 AT 22:42This is one of those rare medical hacks that actually feels like magic. I’ve seen patients on azathioprine turn into walking liver warnings, then after LDAA? They’re hiking, cooking, even going back to work. It’s not just science-it’s a second chance. And the dose drop? From 150mg to 50mg? That’s not cutting corners, that’s cutting the noise so the signal can sing.
My cousin was told to stop everything. Now she’s been stable for 4 years. No liver spikes, no hospital trips. Just quiet, normal life. Doctors need to talk about this more.
Also, allopurinol is basically the wingman of the immunosuppressant world. Low-key, doesn’t ask for credit, just makes everything work better.
Also also-why isn’t this in every IBD protocol yet? It’s cheap, it’s proven, and it saves people from being stuck on steroids forever. We’re not talking fringe stuff here. This is precision medicine doing its damn job.
Melodie Lesesne
January 18, 2026 AT 04:54I love how this works. It’s like your body was trying to burn the gas in the wrong engine, and allopurinol just switched the fuel line. Simple, elegant, and so much safer than just pulling the plug on azathioprine.
My rheumatologist brought this up when I was about to quit my med. I was scared, but after 3 months, my labs looked like a newborn’s. No more nausea, no more liver panic. Just… better.
Also, the fact that you can use this even if you’re TPMT normal? That’s wild. It’s not just for hypermethylators anymore.
Corey Sawchuk
January 19, 2026 AT 06:24LDAA works. I’ve seen it. But don’t skip the labs. I know someone who thought they were fine after a month and didn’t get their 6-TGN checked. Ended up with neutropenia. Scary stuff.
Just because it’s clever doesn’t mean it’s foolproof. Monitor. Monitor. Monitor.
Stephen Tulloch
January 20, 2026 AT 22:01Oh wow another ‘magic combo’ that’s been around since the 90s and still only used by like 3% of GI docs 🙄
Of course it works. You block the bad pathway and force the good one. Duh. Why are we still treating this like it’s a breakthrough? It’s basic pharmacokinetics.
Also 6-MMP >5700? That’s not ‘high’ that’s ‘your liver is screaming.’ Why are we even debating this? 😒
Also also-why do people still think azathioprine is first-line? Just give them anti-TNFs and be done with it. But nooo, let’s keep throwing ancient purines at people like it’s 1987.
Anyway. LDAA is cool. But we need to stop acting like it’s some secret society trick. It’s just good medicine. 🤷♂️
Henry Ip
January 21, 2026 AT 06:43Big respect to the docs who actually track these metabolites. Most just see ‘liver enzymes up’ and say ‘stop the drug.’
But this? This is why I believe in medicine. Not flashy new drugs. Just smart tweaks to old ones.
And yes, the dose drop is everything. 50mg isn’t ‘low dose’-it’s ‘correct dose’ when allopurinol’s in the mix.
Also-patients need to know this exists. No one tells you this is an option until you’re already in crisis.
Kasey Summerer
January 22, 2026 AT 15:47So let me get this straight: we’re using a gout drug to fix a drug that was supposed to fix autoimmune stuff... by redirecting a pathway we didn’t even know existed until the 90s?
Man. Medicine is just one big game of Jenga and we’re all just hoping the tower doesn’t fall.
Also I just used allopurinol to make my beer taste better. Kidding. Or am I? 🍻
Cheryl Griffith
January 23, 2026 AT 21:04I had a friend who was on azathioprine for 3 years and kept getting sick. No one could figure out why. Then someone suggested checking metabolites. Turns out her 6-MMP was through the roof. They put her on LDAA. Within 6 weeks, her energy came back. She started painting again. She’d been too tired to hold a brush for years.
It’s not just about labs. It’s about getting your life back.
Also, the fact that this combo costs less than a monthly Netflix subscription? That’s wild. We should be screaming about this from rooftops.
Corey Chrisinger
January 24, 2026 AT 12:54There’s a quiet poetry here. We’re not curing disease-we’re redirecting chaos. Azathioprine is a wild horse. Allopurinol is the bridle. And 6-TGN? That’s the path home.
It’s not just biochemistry. It’s a metaphor for how we fix broken systems: not by replacing them, but by closing the wrong doors so the right ones can open.
Also, why do we still call it ‘off-label’ when it’s in every major journal? Language is weird. We call wisdom ‘experimental’ until it’s too late to change.
Bianca Leonhardt
January 24, 2026 AT 21:32People still use azathioprine? At all? 🤦♀️
It’s like driving a Model T while Tesla’s on the highway. LDAA? Fine. But why not just go straight to vedolizumab or ustekinumab? This is just delaying the inevitable.
And if you’re relying on metabolite levels, you’re already in the 1% of patients who get real care. Most docs don’t even know what 6-TGN is.
Stop romanticizing outdated protocols. This isn’t innovation. It’s damage control with extra steps.
Travis Craw
January 26, 2026 AT 17:46my doc put me on this and i was scared but it worked so good
no more liver thingys
also allopurinol makes me kinda sleepy but i dont care
still alive so thats good
Christina Bilotti
January 27, 2026 AT 16:00Of course this works. You take a drug that’s metabolized by a single enzyme pathway and block the off-ramp. Shocking, I know.
But the real question is: why are we still using azathioprine at all? It’s a 1960s drug with a 50% failure rate. This isn’t a ‘smart combo’-it’s a band-aid on a broken foundation.
And if you’re not testing 6-TGN and 6-MMP before prescribing, you’re not a doctor-you’re a lottery ticket vendor.
Also, allopurinol? Cute. But if you’re going to go this route, why not just use mycophenolate? It’s safer, easier, and doesn’t require a PhD in pharmacokinetics to manage.
TL;DR: This is clever, but it’s not the future. It’s the last gasp of a dying era.
brooke wright
January 28, 2026 AT 14:16Wait so if I’m on this combo can I still drink? Like one beer? I’m not asking for me I’m asking for a friend. Also my cousin’s mom tried this and now she’s on a cruise and says she feels 20 again. Is that real? Also can you get this in Canada? I’m in Florida and my doctor says no but my cousin’s doctor in Toronto says yes. Also my dog has IBD can I give him allopurinol? Just wondering. Thanks.
Joie Cregin
January 29, 2026 AT 13:14For real though-this is why I love medicine. Not the flashy new biologics. Not the $100k/year drugs. But the quiet, smart, low-cost fixes that actually work.
LDAA isn’t sexy. No one’s making a Netflix doc about it. But it’s the reason someone’s still here to watch their kid graduate. To bake cookies. To hug their partner after a bad day.
And if your doctor hasn’t mentioned this? Ask. Politely. But ask.
It’s not magic. It’s math. And math doesn’t lie.
Also-yes, you can drink. One beer. Maybe two. But don’t test it. Your liver already did enough.