Every year, thousands of people end up in the hospital not because their medicine didn’t work, but because something they ate, drank, or took as a supplement made it work too well-or not at all. It’s not magic. It’s chemistry. And it’s happening right now, in kitchens, medicine cabinets, and pharmacies across the country. You might be taking warfarin for your heart, sipping grapefruit juice with breakfast, and popping a St. John’s wort capsule for mood support. None of that sounds dangerous. But together? That combo can send your INR sky-high, cause internal bleeding, or make your blood thinner useless. This isn’t a rare accident. It’s predictable. And it’s preventable.
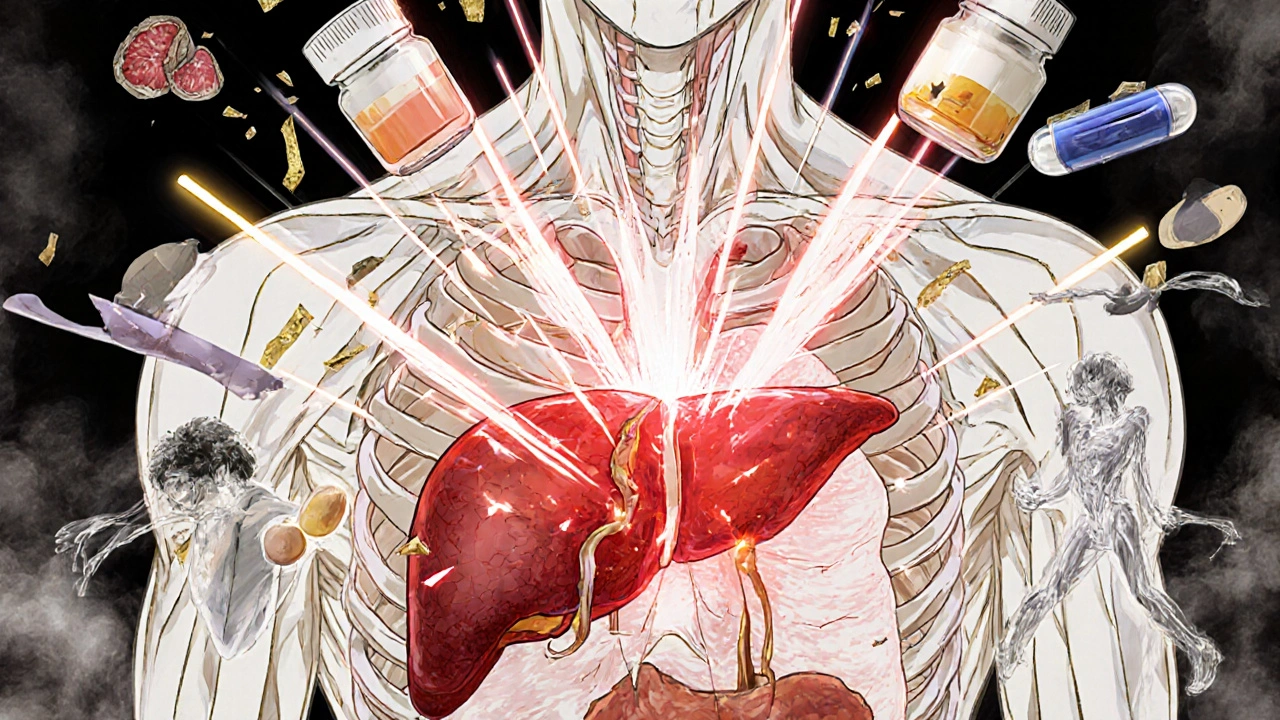
How Drug Interactions Actually Work
Drug interactions aren’t just about pills clashing. They’re about your body’s systems being hijacked. There are two main ways this happens: pharmacodynamic and pharmacokinetic.
Pharmacodynamic interactions happen when two substances have similar or opposite effects on your body. Take hawthorn, a popular heart supplement. It boosts heart muscle contraction. Now add digitalis, a common heart failure drug that does the same thing. Together? Your heart gets overstimulated. You could develop dangerous irregular rhythms or even heart failure. On the flip side, yohimbine (found in some energy supplements) blocks the same receptors as guanabenz, a blood pressure drug. One tries to lower your pressure. The other fights it. Result? Your blood pressure stays high, even though you’re taking your meds.
But the bigger threat? Pharmacokinetic interactions. These mess with how your body absorbs, breaks down, or gets rid of drugs. The liver is ground zero. The cytochrome P450 enzyme system-especially CYP3A4-handles about half of all prescription medications. When something like St. John’s wort triggers this system, your body starts breaking down drugs faster. That means less medicine in your bloodstream. Cyclosporine, used after organ transplants, can drop by 70% in just two weeks. That’s not a side effect. That’s transplant rejection waiting to happen.
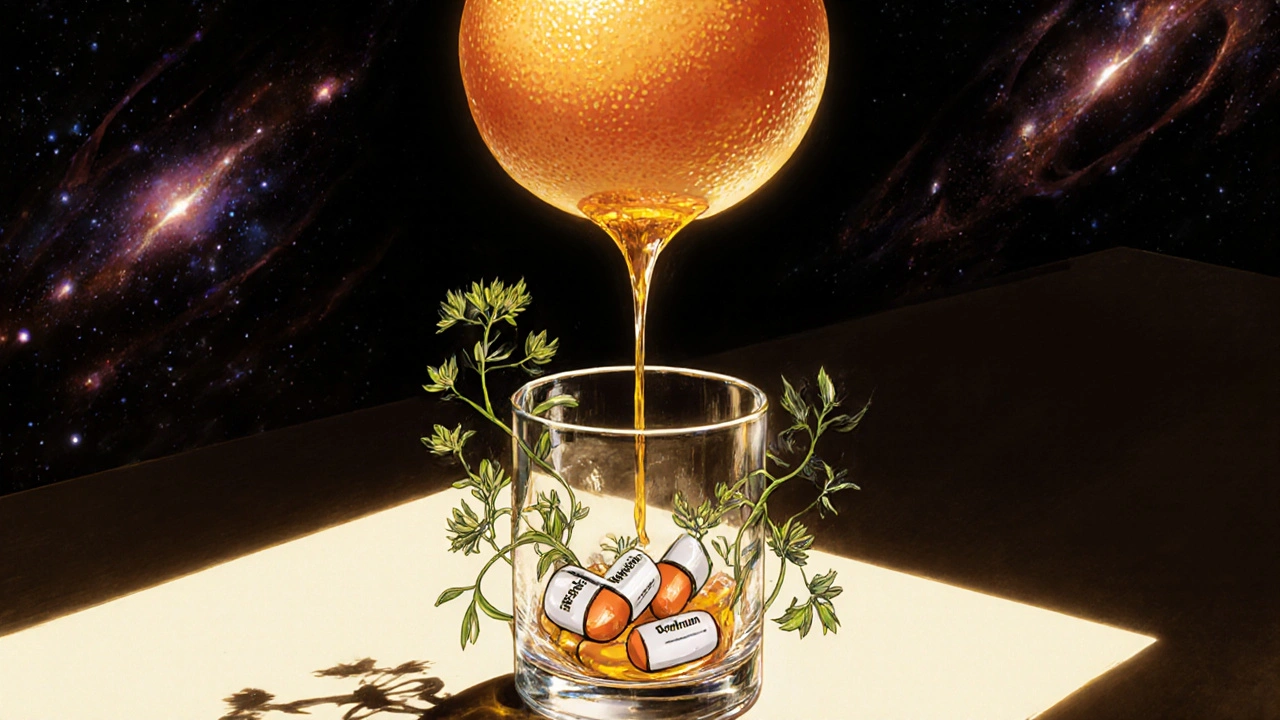
Grapefruit Isn’t Just a Fruit-It’s a Drug Saboteur
People think grapefruit is healthy. It is. But it’s also one of the most dangerous things you can eat if you’re on certain meds. The problem? Furanocoumarins. These natural compounds in grapefruit (and pomelo, Seville oranges) permanently disable the CYP3A4 enzyme in your gut. That enzyme normally breaks down drugs before they enter your bloodstream. Without it? Your body absorbs way more than intended.
Take simvastatin, a common cholesterol pill. Normally, your body absorbs about 5% of it. With grapefruit? That jumps to 70%. That’s a 15-fold increase. The result? Muscle breakdown-rhabdomyolysis. This isn’t just soreness. It’s your muscles dissolving. That releases toxins into your blood, which can shut down your kidneys. The risk goes from 0.15 cases per 100,000 people a year to 1.57. That’s a 10x spike. And it doesn’t take much. One glass of grapefruit juice, eaten hours before your pill, is enough. The effect lasts over 24 hours. So even if you drink it at breakfast and take your pill at night? Still risky.
Supplements Are Not Always Safe-Even When They’re Natural
"Natural" doesn’t mean harmless. In fact, it often means less tested. The Dietary Supplement Health and Education Act of 1994 let supplements hit shelves without proving safety or effectiveness. That’s why you’ll find ginkgo biloba on the shelf next to aspirin, with no warning labels. But ginkgo thins your blood. So does aspirin. Together? Your bleeding risk shoots up. Studies show ginkgo can prolong bleeding time by 30-50%. In one case, a 72-year-old man on warfarin started taking ginkgo for memory. Two weeks later, he had a brain bleed. He survived. But only because his wife noticed he was unusually tired and took him in.
Garlic supplements? Same story. A 2001 study found 32 cases of serious bleeding when garlic was mixed with warfarin, heparin, or aspirin. Red yeast rice? It contains lovastatin-a prescription statin. Taking it with simvastatin or atorvastatin? You’re doubling your statin dose. That raises your risk of muscle damage by 2.3 times. Coenzyme Q10? It might make your statins less effective. You take it hoping to protect your heart. Instead, you might be undoing the benefit of your actual heart medicine.
And then there’s St. John’s wort. It’s marketed for mild depression. But it doesn’t just affect serotonin. It turns on CYP3A4 like a faucet. It can slash levels of birth control pills by 50-70%. That’s not a myth. That’s documented pregnancy. It drops HIV meds by 40-80%. That’s not just treatment failure-it’s drug-resistant virus. And when mixed with SSRIs like sertraline or fluoxetine? You risk serotonin syndrome: high fever, shaking, confusion, rigid muscles. It can kill you in hours.
Vitamin K: The Silent Saboteur in Your Salad
If you’re on warfarin, your doctor probably told you to avoid leafy greens. That’s outdated advice. The real rule? Keep your intake consistent. A sudden spike in vitamin K-like eating a big bowl of cooked spinach (830mcg)-can drop your INR by 30-40% in a day. That means your blood clots faster. You’re at risk for stroke or pulmonary embolism.
But if you eat spinach every day? Your body adjusts. Your INR stays stable. That’s why the FDA and National Academy of Medicine recommend 90mcg daily for women and 120mcg for men. Not zero. Just steady. Same goes for green tea, broccoli, and Brussels sprouts. You don’t need to cut them out. Just don’t start eating them like you never have before.
Cranberry juice? That’s another myth. Yes, there were 28 case reports of bleeding between 2003 and 2015. But most were in older people on high-dose warfarin. The risk is real-but not universal. Still, if you’re on warfarin and you drink cranberry juice daily, tell your doctor. Don’t assume it’s fine.
What You Can Do Right Now
Most people don’t tell their doctor about supplements. A 2022 JAMA study found 70% of patients keep quiet. Why? They think it’s not medicine. Or they’re afraid their doctor will judge them. But your doctor isn’t here to scold you. They’re here to keep you alive.
Here’s what to do:
- Make a complete list. Write down every pill, capsule, tea, tincture, and vitamin you take-even the ones you only use once a month. Include OTC meds like ibuprofen or antacids.
- Bring it to every appointment. Don’t just say, “I take a multivitamin.” Say: “I take Nature Made Multi 50+, 1000 IU vitamin D, ginkgo biloba 120mg, and fish oil 1000mg.” Be specific.
- Ask your pharmacist. They’re the drug experts. Most pharmacies offer free medication reviews. Ask: “Does this interact with anything I’m on?” They’ll check against 3,500+ drugs and supplements.
- Use free tools. Go to MedlinePlus.gov. Type in your drug and supplement. It’ll tell you if there’s a known interaction, how serious it is, and what to watch for.
- Don’t start or stop anything without asking. Even if it’s “just a herbal tea.”

Why This Matters More Than Ever
Over 40% of American adults take supplements. That’s 130 million people. And the FDA says 23% of serious supplement-related hospitalizations are due to interactions. That’s not a small number. That’s 30,000 people a year-just in the U.S.
And it’s getting worse. Supplement sales hit $50 billion in 2024. Labels still don’t have interaction warnings. Only 29% of them do. Prescription drugs? 100% do. Why? Because supplements aren’t regulated like drugs. But your body doesn’t care. It treats them the same.
There’s hope. AI tools like IBM Watson Health are now scanning millions of medical notes to predict new interactions. Hospitals are using electronic systems that flag risky combos before a doctor even writes the script. In one study, that cut high-risk prescriptions by 37%.
But technology won’t save you if you don’t speak up. The most powerful tool you have is your voice. Tell your doctor. Tell your pharmacist. Write it down. Keep it updated. Because when it comes to your meds, what you eat, drink, or swallow matters more than you think.
When to Seek Help Immediately
If you’re on any of these meds and start feeling off after changing your diet or starting a supplement, get help fast:
- Warfarin: Unexplained bruising, nosebleeds, blood in urine or stool, severe headaches.
- Statins: Unusual muscle pain, weakness, dark urine (sign of muscle breakdown).
- SSRIs or St. John’s wort: High fever, fast heartbeat, confusion, muscle stiffness, seizures.
- Immunosuppressants (like cyclosporine): Fever, chills, swelling, signs of organ rejection.
These aren’t side effects. They’re emergencies.
Can I still drink grapefruit juice if I take a statin?
No-not if you’re taking simvastatin, atorvastatin, or lovastatin. Grapefruit juice can increase these drugs’ levels by up to 15 times, raising your risk of muscle damage and kidney failure. If you’re on rosuvastatin or pravastatin, grapefruit is generally safe. But always check with your pharmacist. There’s no safe amount if you’re on the wrong statin.
Is St. John’s wort safe for depression if I’m not on other meds?
Even if you’re not on other medications, St. John’s wort isn’t risk-free. It can cause sun sensitivity, anxiety, dizziness, and digestive issues. It’s not regulated, so potency varies. Studies show it works for mild depression-but only as well as a placebo for moderate cases. If you’re considering it, talk to a doctor first. There are safer, proven options.
Do all supplements interact with medications?
No. Many don’t. But you can’t assume any are safe. Ginkgo, garlic, ginseng, echinacea, and high-dose vitamin E are known risks. Multivitamins are usually fine unless they contain mega-doses of vitamin K, vitamin E, or iron. The key is knowing what’s in your supplement. Read the label. If you’re unsure, ask a pharmacist.
Why don’t supplement labels have interaction warnings like prescription drugs?
Because they’re not required to. Under the 1994 DSHEA law, supplements are treated as food, not drugs. That means manufacturers don’t need FDA approval before selling them-and they don’t need to prove safety or interaction risks. Only 29% of labels include warnings. That’s why it’s up to you to research and ask questions.
Can my pharmacist check all my meds and supplements for interactions?
Yes. Pharmacists have access to databases with over 3,500 drugs and supplements. They can check for interactions between your prescriptions, OTC meds, vitamins, and herbal products. Many pharmacies offer this service for free. Bring your list-even the bottle caps-to your next visit. It takes 10 minutes. It could save your life.
What if I forgot to tell my doctor about a supplement I started?
Tell them the next time you see them. Don’t wait. Don’t feel embarrassed. Most doctors have seen this before. They’ve treated people who took ginkgo with warfarin, St. John’s wort with antidepressants, or garlic with blood thinners. The sooner you speak up, the sooner they can adjust your treatment. If you’re worried about a reaction right now, call your doctor or go to urgent care.
If you’re taking any prescription medication, your body is a complex system. Food, supplements, and drugs don’t just sit beside each other-they talk. And sometimes, they argue. Your job isn’t to know every interaction. Your job is to make sure the right people know what you’re taking. That’s how safety starts.


Evan Brady
November 18, 2025 AT 10:48St. John’s wort isn’t just a ‘natural remedy’-it’s a biochemical sledgehammer. It induces CYP3A4 and P-glycoprotein like a rogue thermostat cranking up your liver’s detox mode. That’s why your birth control fails, your cyclosporine tanks, and your SSRIs turn into placebo candy. No mysticism. Just pharmacokinetics. And yes-it’s on the FDA’s radar. But nobody reads the fine print until someone’s in the ER with serotonin syndrome.
Kevin Jones
November 19, 2025 AT 08:54Pharmacokinetics > placebo effect. The liver doesn’t care if it’s ‘natural.’ CYP3A4 is the gatekeeper-and grapefruit? It’s the bouncer with a sledgehammer. One glass. 24 hours. Permanent enzyme inhibition. Simvastatin levels don’t ‘go up’-they explode. Muscle dissolution isn’t a side effect. It’s a chemical betrayal.
mithun mohanta
November 20, 2025 AT 03:55Of course the FDA doesn’t regulate supplements-because the pharmaceutical cartel owns the regulatory apparatus. They want you dependent on pills they patent, not on turmeric or garlic that cost pennies. This whole ‘interaction’ narrative? A distraction. The real danger? Corporate greed disguised as science. Wake up.
Premanka Goswami
November 20, 2025 AT 04:32They told you grapefruit was healthy. They told you ‘natural’ meant safe. They lied. The FDA, Big Pharma, the WHO-they all profit from your ignorance. St. John’s wort? It’s been banned in 12 countries. Why? Because it exposes the fragility of their chemical empire. They don’t want you to know you can heal without their patents. This isn’t medicine. It’s control.
Brandon Lowi
November 21, 2025 AT 12:39Let’s be clear: if you’re taking supplements and not screaming into the void about Big Pharma’s lies, you’re part of the problem. This isn’t about ‘interactions’-it’s about the U.S. government letting corporations poison you with impunity. Ginkgo? Garlic? They’re ancient remedies. The system fears them. So they bury the data. And you? You’re just a walking profit margin.
Joshua Casella
November 21, 2025 AT 22:22I’ve been a pharmacist for 18 years. I’ve seen 72-year-olds bleed out because they took ginkgo with warfarin and thought ‘it’s just herbs.’ I’ve seen transplant patients reject organs because they drank grapefruit juice with cyclosporine. I’ve seen people on SSRIs end up in ICU from St. John’s wort. This isn’t theoretical. It’s daily. If you take anything-even a multivitamin-bring it to your pharmacist. No judgment. Just safety.
Alex Boozan
November 23, 2025 AT 05:28It’s not about ‘interactions.’ It’s about sovereignty. Your body is a biological network. Supplements, food, meds-they’re all signals. And the system is rigged to make you dependent on patented molecules. The fact that grapefruit disables CYP3A4? That’s a gift. Nature’s way of saying: ‘You don’t need their drugs.’ But they’ll never let you know that. Because control is more profitable than health.
Saket Sharma
November 24, 2025 AT 02:31Anyone who thinks ‘natural’ equals safe is either delusional or complicit. Ginkgo? Blood thinner. Garlic? Blood thinner. Red yeast rice? Hidden statin. CoQ10? Statin neutralizer. And you’re just ‘taking vitamins’? You’re playing Russian roulette with your liver, kidneys, and heart. The only ‘natural’ thing here? Your ignorance. Educate yourself-or die quietly.
Richard Couron
November 25, 2025 AT 22:25They don’t want you to know this. They don’t want you to know that your ‘healthy’ green smoothie with spinach and ginkgo is sabotaging your warfarin. They don’t want you to know that your ‘natural’ mood booster is killing your HIV meds. They profit from your silence. So you keep drinking grapefruit juice. You keep popping St. John’s wort. And you wonder why you’re sick. It’s not bad luck. It’s corporate malice.
Shravan Jain
November 26, 2025 AT 04:43the cyp3a4 enzyme system is overrated. most interactions are overstated. i’ve been on 12 meds and 7 supplements for 8 years. never had an issue. you people are just scared of the word ‘natural.’ science is not a religion. stop fearmongering. also, vitamin k in spinach? chill. your INR fluctuates anyway. just test weekly.
Alexis Paredes Gallego
November 27, 2025 AT 02:53They say ‘consult your doctor.’ But your doctor doesn’t know anything. They were trained by Pharma. They don’t know that St. John’s wort blocks SSRIs. They don’t know grapefruit disables CYP3A4. They don’t even know what ‘pharmacokinetic’ means. They just prescribe. And you? You’re the lab rat. Wake up. The system is designed to fail you. Your only hope? Stop trusting anyone with a white coat.
Ram tech
November 27, 2025 AT 11:55why are you even reading this? just take your pills. dont mix stuff. dont eat greens. dont drink juice. dont take supplements. life is simple. dont be smart. be safe. also, who cares about cyp3a4? just go to doc. they know better. i trust them.