Every year, thousands of children are given the wrong dose of medicine-not because someone was careless, but because a simple number got lost in translation. A weight written in pounds instead of kilograms. A calculation done on a napkin. A scale that doesn’t show decimals. These aren’t rare mistakes. They’re systemic failures-and they’re preventable.
Why Weight-Based Checks Are Non-Negotiable in Pediatric Care
Children don’t get adult doses. Their bodies process medicine differently. A dose that’s safe for a 70-kilogram teen could be lethal for a 5-kilogram infant. That’s why every pediatric medication must be calculated by weight, usually in milligrams per kilogram (mg/kg). The math isn’t hard. But the margin for error is razor-thin.The World Health Organization says children are three times more likely than adults to suffer a medication error. Why? Because weight-based dosing requires precision. One wrong decimal. One misread scale. One outdated weight in the system. That’s all it takes.
A 2021 review of 63 studies found that over 32% of pediatric dispensing errors involved incorrect weight-based calculations. Nearly 9% of those led to actual harm-slow breathing, seizures, organ damage. And the CDC found that 40% of liquid medication errors in kids under four came from pounds-to-kilograms mix-ups. That’s not a glitch. That’s a design flaw.
The Three Critical Points of Verification
Preventing these errors isn’t about one magic tool. It’s about three non-negotiable checkpoints where weight is verified-every single time.- Prescription Entry: The doctor or nurse must enter the child’s current weight in kilograms before the system will allow a prescription to be submitted. No weight? No order. This isn’t optional. The American Society of Health-System Pharmacists (ASHP) made this mandatory in 2018.
- Pharmacy Verification: The pharmacist doesn’t just fill the script. They double-check the weight, the dose, and the math. If the EHR doesn’t auto-calculate, they do it by hand-and they sign off on it. Studies show pharmacist-led verification cuts administration errors by over 15 percentage points.
- Bedside Administration: Before the medicine goes in, the nurse scans the barcode, confirms the patient’s weight in the system, and verifies the dose matches the calculated amount. This step alone reduces errors by 74%.
Dr. Matthew Grissinger from the Institute for Safe Medication Practices calls this the "triple-check rule." Skip any one of these steps, and you’re gambling with a child’s life.
Technology That Actually Works
You can’t rely on people to be perfect. But you can build systems that make mistakes harder to make.Electronic Health Record (EHR) systems with built-in clinical decision support (CDSS) are the backbone of modern safety. These systems don’t just remind you to enter weight-they block you from prescribing outside safe ranges. A 2022 study showed EHR-integrated CDSS reduced dosing errors by 87% when configured correctly.
But not all systems are equal. Some trigger too many alerts. Pharmacists on Reddit report that Epic EHR often flags doses as "too high" for teens who are close to adult weight-even when the dose is correct. That’s alert fatigue. And when alerts become noise, people start ignoring them. In one study, 42% of weight-based alerts were overridden-and 18% of those overrides were actual errors.
That’s why the latest tools are smarter. Epic’s Pediatric Safety Module 4.0, released in January 2024, uses growth percentiles instead of fixed weight thresholds. If a child’s dose falls outside their expected range based on age and past growth, it flags it-not because the number is wrong, but because it’s unusual. This cut inappropriate alerts by over 60% in testing.
Automated dispensing cabinets with weight verification cut errors by nearly 70%. But they add 2.3 minutes per prescription. That’s a trade-off. Hospitals that cut corners here end up with faster workflows but higher risks.
How Weights Are Measured-and Why It Matters
The scale matters as much as the math.The American Academy of Pediatrics says all pediatric scales must display weight in kilograms only. No pounds. No ounces. No "18 lbs" typed into a computer. Why? Because humans mess up conversions. One study found that 12.6% of pediatric dosing errors came from pounds-to-kilograms mistakes.
Infants need scales accurate to 0.1 kg. Toddlers and older kids? 0.5 kg is enough. But if the scale shows pounds, or if staff are used to eyeballing weights, errors creep in. A 2022 survey of 1,247 pediatric nurses found that 63% had seen weight documentation errors in the past year. Over 40% said those errors caused delays in giving medicine.
And outdated weights? They’re deadly. The ISMP says weights must be measured within 24 hours for acute care patients and within 30 days for outpatients. If a child was weighed last month and now weighs 2 kg more, that dose is no longer safe.
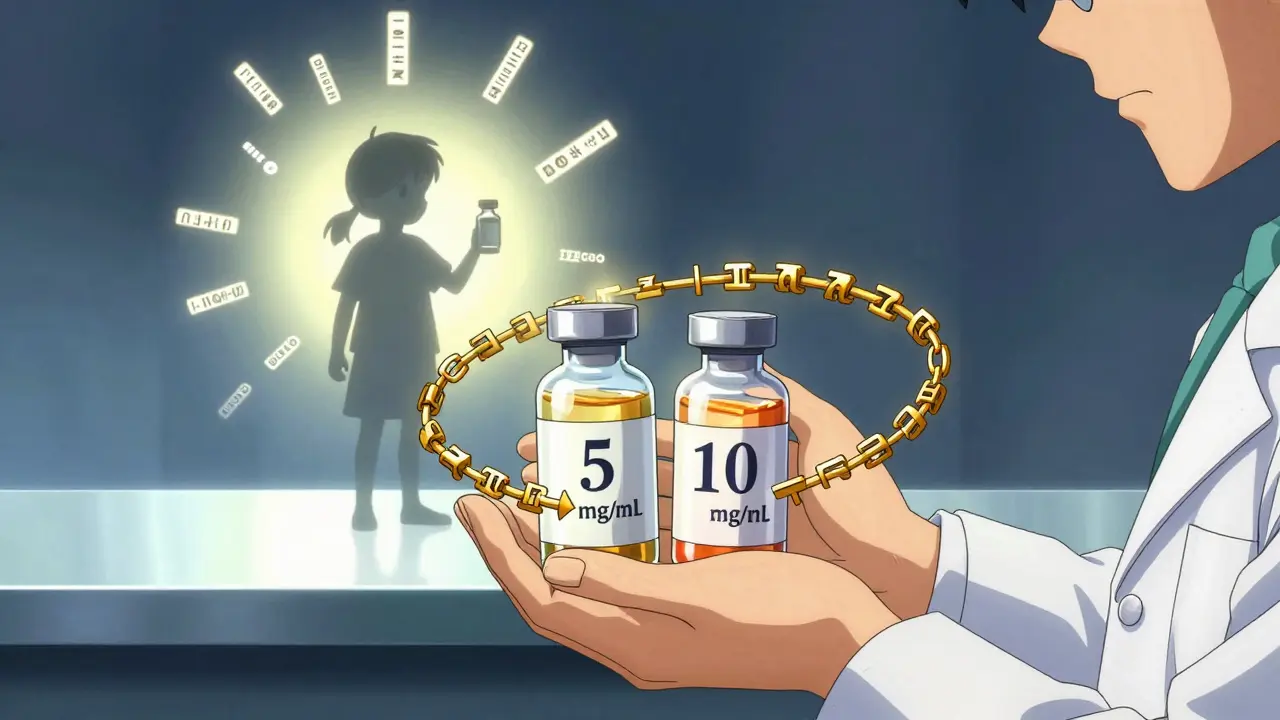
Standardizing Concentrations Saves Lives
Another silent killer? Variable drug concentrations.Imagine two different bottles of vancomycin-one is 5 mg/mL, another is 10 mg/mL. A nurse grabs the wrong one. The dose doubles. That’s not hypothetical. It’s happened.
Facilities that standardize concentrations-using the same strength for common pediatric meds across all units-cut calculation errors by 72%. That’s not a nice-to-have. It’s a safety baseline. The ASHP recommends it. The CDC supports it. Yet many hospitals still use multiple concentrations because it’s "tradition."
The Real Barriers to Implementation
You’d think everyone would have this figured out by now. But they haven’t.68% of hospitals say their EHR systems don’t talk well to each other. If the ER’s weight isn’t synced to the ICU’s system, the nurse is working with old data. That’s a gap.
41% of doctors say weight entry slows them down. They don’t want to stop typing to find the weight field. That’s a workflow problem. And 38% of pharmacy staff haven’t had proper training on pediatric pharmacokinetics. They know how to count pills. They don’t know how kids metabolize drugs differently.
And then there’s the rural divide. 94% of children’s hospitals have full weight verification systems. Only 33% of rural community hospitals do. That means kids in small towns are 3 times more likely to get a wrong dose than kids in big cities.
What Success Looks Like
Boston Children’s Hospital made a simple change: they required weight to be entered in kilograms only. Within 18 months, weight conversion errors dropped from 14.3 per 10,000 doses to 0.8. That’s a 94% reduction.They also added a pharmacist verification step before every pediatric dose. The cost? 37% longer verification time. The benefit? Zero preventable deaths from dosing errors.
Other hospitals followed. The Leapfrog Group now requires weight verification for a top "A" safety rating. CMS now demands it for Medicare/Medicaid claims. The market for pediatric safety tech is projected to hit $2.3 billion by 2027.
But technology alone won’t fix this. As Dr. Robert Wachter from UCSF says, "A culture of safety with non-punitive error reporting is essential." If a nurse is afraid to speak up when something looks wrong, the system fails-even if it’s perfect.
What You Can Do Right Now
If you’re a clinician, pharmacist, or administrator:- Check your EHR: Does it require weight entry before prescribing? If not, push for it.
- Verify weight at every handoff: admission, pharmacy, bedside. No exceptions.
- Switch all scales to kilograms only. Remove pound displays.
- Standardize concentrations for common pediatric meds. No more "it depends on the unit."
- Train staff on pediatric pharmacokinetics-not just dosing math, but how kids process drugs differently.
- Review weights every 24 hours for inpatients. Every 30 days for outpatients.
- Encourage reporting. If someone catches a near-miss, thank them. Don’t punish them.
Preventing pediatric dispensing errors isn’t about being perfect. It’s about building layers of protection so that when one fails, another catches it. Weight-based checks are the most powerful layer we have. Use them. Every time. No exceptions.



Praseetha Pn
January 18, 2026 AT 02:32Joni O
January 19, 2026 AT 06:56Robert Cassidy
January 20, 2026 AT 00:54Max Sinclair
January 20, 2026 AT 02:12Wendy Claughton
January 22, 2026 AT 01:58Ryan Otto
January 22, 2026 AT 03:23Tyler Myers
January 23, 2026 AT 13:18Emma #########
January 23, 2026 AT 23:32Nishant Sonuley
January 25, 2026 AT 19:48Andrew Short
January 25, 2026 AT 22:51Andrew McLarren
January 27, 2026 AT 09:43