For decades, proving that a generic drug works the same as the brand-name version meant putting healthy volunteers through blood draws, fasting periods, and long clinic visits. These in vivo bioequivalence studies cost up to $2 million each and took months to complete. But now, a smarter, faster approach is changing the game: in vitro testing backed by IVIVC. It’s not science fiction-it’s the new standard for complex generics, and it’s saving the industry millions while reducing patient burden.
What Is IVIVC, Really?
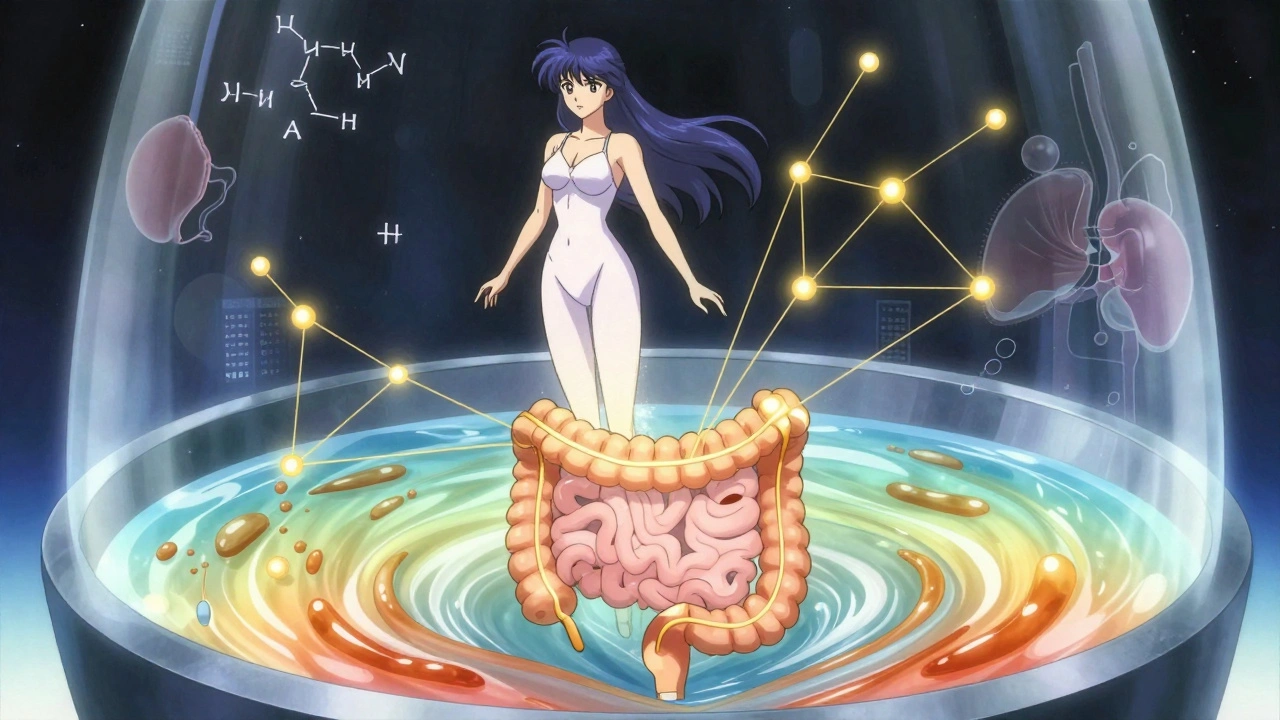
IVIVC stands for In Vitro-In Vivo Correlation. At its core, it’s a mathematical model that links what happens in a lab dish to what happens inside the human body. Specifically, it connects how fast a drug dissolves in a test solution (in vitro) to how quickly and completely that drug gets absorbed into the bloodstream (in vivo).This isn’t just about dissolving a pill in water. It’s about replicating the messy, dynamic environment of the gut-pH changes, bile salts, stomach emptying times. When done right, a well-built IVIVC model can predict a drug’s entire pharmacokinetic profile from a single dissolution test. That means no more human trials for minor formulation tweaks.
The U.S. FDA first laid out the rules in 1996, but it wasn’t until the 2014 guidance that the framework became clear enough for companies to build reliable models. The European Medicines Agency followed with similar standards. Today, if you can prove a strong IVIVC, regulators may let you skip the human study entirely-a biowaiver.
The Four Levels of IVIVC: Not All Correlations Are Equal
Not every IVIVC is created equal. The FDA classifies them into four levels, and only one really unlocks full biowaiver power.- Level A: The gold standard. It’s a point-to-point match between dissolution at every time point and absorption at every time point. Think of it like a perfect mirror: if the drug dissolves 40% at 1 hour, absorption should be exactly 40% too. Acceptable models need R² > 0.95, slope near 1.0, and intercept near zero. This is the only level that allows full waivers for post-approval changes.
- Level B: Uses average values-mean dissolution time versus mean residence time. It’s useful for trends, but can’t predict individual profiles. Not enough for waivers.
- Level C: Links one dissolution number (like % dissolved at 30 minutes) to one pharmacokinetic number (like Cmax). Limited. Sometimes accepted if backed by extra data.
- Multilevel C: Multiple Level C points strung together. Better than single C, but still not as reliable as Level A. Regulators are cautious.
For any waiver request, Level A is the target. If you’re aiming for a biowaiver, you’re not just building a correlation-you’re building a predictive engine.
Why IVIVC Beats In Vivo Testing-When It Works
The math is simple: one in vivo bioequivalence study costs $500,000 to $2 million and requires 24-36 volunteers. That’s a huge barrier for generic manufacturers, especially when you need to test multiple formulations or make small changes after approval.With a validated IVIVC, you can:
- Replace 3-5 bioequivalence studies for post-approval changes like manufacturing scale-up or minor excipient adjustments
- Reduce development time by 6-12 months
- Save $1-2 million per avoided study
Take Teva’s extended-release oxycodone generic. They spent 14 months and three formulation tries to nail their Level A IVIVC. But once approved, they avoided five future bioequivalence studies. That’s over $10 million saved.
And it’s not just about money. Fewer human trials mean less burden on volunteers, faster access to affordable medicines, and less strain on clinical trial infrastructure.
Why Most IVIVC Submissions Fail
Despite the clear benefits, only about 42% of IVIVC submissions get approved today-up from 15% in 2018, but still low. Why?According to FDA reviews of 127 submissions in 2023, the top three reasons for rejection are:
- Poor physiological relevance (64%): The dissolution test didn’t mimic the real gut. Using plain water or a single pH? That’s outdated. Biorelevant media-containing bile salts, enzymes, and pH gradients-are now required for complex products.
- Inadequate formulation space (28%): You can’t build a model with just two formulations. You need at least three: fast-releasing, medium, and slow-releasing. Without this range, the model can’t predict behavior across real-world variations.
- Weak validation (22%): The model looked good on paper but failed when tested against new data. Validation isn’t a checkbox-it’s a rigorous process using independent datasets.
One company spent $1.2 million over 18 months on an IVIVC for a modified-release product-only to see it collapse when food effects were added. The model didn’t account for real-life variability. That’s why experts say: “Don’t build an IVIVC to get a waiver. Build it because you understand your drug.”
When IVIVC Doesn’t Work-And What to Use Instead
IVIVC isn’t magic. It has hard limits.For immediate-release drugs with high solubility and permeability (BCS Class I), regulators accept simple BCS-based biowaivers. No IVIVC needed. Just prove the drug dissolves quickly and is well-absorbed.
But for extended-release, complex injectables, or ophthalmic products, IVIVC is often the only viable path. Even then, it fails for:
- Narrow therapeutic index drugs (like warfarin or digoxin)-where tiny differences matter
- Drugs with nonlinear absorption or metabolism
- Products with poor solubility or erratic gastric emptying
In these cases, in vivo studies are still mandatory. The FDA won’t risk patient safety for convenience.
The Rise of Biorelevant Dissolution and Machine Learning
The future of IVIVC isn’t in old-school dissolution apparatuses. It’s in biorelevant media that mimic the human GI tract.University of Maryland research shows that adding bile salts and adjusting pH gradients can improve correlation accuracy by 40%. The FDA now expects this for any complex product submission. By 2025, 75% of new IVIVC submissions will use biorelevant methods, according to the American Association of Pharmaceutical Scientists.
And now, machine learning is entering the picture. In 2024, FDA and EMA held a joint workshop on AI-enhanced IVIVC models. Companies are training algorithms to find hidden patterns in dissolution and pharmacokinetic data-something humans might miss.
But here’s the catch: AI models must be transparent. Regulators won’t accept a “black box.” You must explain how the algorithm works, what variables it uses, and how it was validated.

Who’s Doing It Right-and Who’s Falling Behind
Large generic manufacturers lead the pack. Only five of the top 10: Teva, Mylan, Sandoz, Sun Pharma, and Lupin, have dedicated IVIVC teams. Why? Because they have the resources: in-house pharmacokinetic experts, access to clinical trial networks, and the budget to fail a few times before succeeding.Smaller companies? They often try once, get rejected, and give up. A 2022 survey of 47 generic firms found that 68% attempted IVIVC, but only 29% succeeded on the first try. Common reasons: not enough pharmacokinetic data, poor dissolution methods, or no expert to run the models.
That’s where contract research organizations (CROs) like Alturas Analytics and Pion come in. Their success rate? 60-70% for Level A models-nearly double the industry average. Why? They specialize in this. They know what the FDA wants before you submit.
What You Need to Build a Successful IVIVC
If you’re serious about IVIVC, here’s the roadmap:- Start early: Don’t wait until the end of development. Begin during Phase 2 trials or prototype formulation.
- Build a formulation space: Create at least three versions-fast, medium, and slow release. Each must be well-characterized.
- Use biorelevant media: No more water. Use FaSSIF, FeSSIF, or other physiological media.
- Collect dense PK data: At least 12 blood time points per subject, across 3-5 studies with 12-24 volunteers each.
- Validate rigorously: Test your model on data it didn’t see during training. Use statistical thresholds: ±10% for AUC, ±15% for Cmax.
- Get expert help: If you don’t have a pharmacokinetic modeler on staff, hire one. This isn’t a task for a junior scientist.
It takes 12-18 months. It’s expensive. But if you’re making complex generics, it’s the only way to compete.
The Future: More Waivers, More Complexity
The trend is clear. By 2027, IVIVC-supported waivers could account for 35-40% of all modified-release generic approvals-up from 22% in 2022. The FDA has allocated $15 million in GDUFA III funding to improve guidance for complex products. New draft guidance on topical products suggests IVIVC is expanding beyond oral drugs.But the real shift isn’t just technical-it’s cultural. Regulators are no longer skeptical. They’re demanding it. If you’re submitting a new extended-release product in 2025 without an IVIVC, you’re already behind.
The future of bioequivalence isn’t more human trials. It’s smarter science. Better models. More accurate predictions. IVIVC isn’t replacing in vivo testing because it’s easier-it’s replacing it because it’s better. And if you’re not building it, you’re not building the future of generics.
What is the main purpose of IVIVC in generic drug development?
The main purpose of IVIVC is to establish a scientifically valid link between how a drug dissolves in a lab test and how it behaves in the human body. When proven strong enough, this allows regulators to waive expensive and time-consuming human bioequivalence studies, speeding up approval and reducing costs without compromising safety.
Can IVIVC be used for all types of drugs?
No. IVIVC works best for oral extended-release products and complex formulations where absorption is predictable. It’s not suitable for drugs with narrow therapeutic indexes (like warfarin), nonlinear pharmacokinetics, or poorly soluble drugs. For immediate-release drugs that are highly soluble and permeable (BCS Class I), simpler biowaivers based on the Biopharmaceutics Classification System are preferred.
Why do most IVIVC submissions get rejected by regulators?
Most rejections happen because the dissolution test doesn’t reflect real human physiology-like using plain water instead of biorelevant media. Other common reasons include not testing enough formulations (need at least three), insufficient pharmacokinetic data, or failing to validate the model on new, unseen data. The FDA requires predictions to be within ±10% for AUC and ±15% for Cmax.
Is IVIVC cheaper than running in vivo bioequivalence studies?
Yes, but only if you succeed. Building a Level A IVIVC costs $1-2 million upfront and takes 12-18 months. But once approved, it can replace 5-10 future bioequivalence studies, each costing $500,000-$2 million. So while the initial investment is high, the long-term savings are massive-often over $10 million per product.
What’s the difference between IVIVC and BCS-based biowaivers?
BCS-based biowaivers apply only to immediate-release drugs that are highly soluble and highly permeable (BCS Class I). They rely on solubility and permeability data alone. IVIVC applies to complex formulations-especially extended-release-where absorption isn’t straightforward. IVIVC requires dissolution testing across multiple formulations and pharmacokinetic data to build a predictive model. BCS is simpler; IVIVC is more powerful but far more complex.
Do I need special training to develop an IVIVC?
Yes. Developing a valid IVIVC requires expertise in pharmaceutics, dissolution methodology, pharmacokinetics, and statistical modeling. Most companies hire specialists with advanced degrees and 2-3 years of experience. Certification programs from the American Association of Pharmaceutical Scientists (AAPS) are available and increasingly expected by regulators.


Pooja Surnar
December 4, 2025 AT 09:08Sandridge Nelia
December 4, 2025 AT 22:06Mark Gallagher
December 5, 2025 AT 18:44Wendy Chiridza
December 5, 2025 AT 22:16Pamela Mae Ibabao
December 7, 2025 AT 19:38Gerald Nauschnegg
December 9, 2025 AT 06:33Palanivelu Sivanathan
December 10, 2025 AT 15:30Joanne Rencher
December 11, 2025 AT 03:11Erik van Hees
December 12, 2025 AT 17:17Cristy Magdalena
December 14, 2025 AT 06:01Adrianna Alfano
December 16, 2025 AT 00:17