Opioid Safety: How to Use Prescription Painkillers Without Risk
When doctors prescribe opioids, a class of powerful pain-relieving drugs that include oxycodone, hydrocodone, and morphine. Also known as narcotics, they can be life-changing for severe pain—but they carry real risks of dependence, overdose, and even death if not handled carefully. Millions of people take them safely every year, but too many don’t know the warning signs or how to respond when things go wrong.
Naloxone, a fast-acting medication that reverses opioid overdoses is now available without a prescription in many places. If you or someone you know takes opioids, having naloxone on hand isn’t just smart—it could save a life. It works in minutes, even if you’re not a medical professional. The CDC recommends keeping it in your medicine cabinet if opioids are part of your treatment plan. But naloxone isn’t a fix for addiction. That’s where prescription opioid guidelines, evidence-based rules doctors follow to limit long-term use and monitor for misuse come in. These guidelines aren’t about denying pain relief—they’re about making sure you get the right dose for the right amount of time.
Opioid safety isn’t just about avoiding overdose. It’s about understanding how these drugs affect your brain, why tolerance builds, and how easily dependence can sneak up on you. People often think addiction only happens to those who abuse drugs, but studies show that even patients taking opioids exactly as prescribed can develop physical dependence within weeks. That’s why regular check-ins with your doctor matter. If your pain improves, ask if you can lower the dose or stop. If you’re taking more than prescribed, or if you’re running out early, that’s a red flag—not a failure, but a signal to talk.
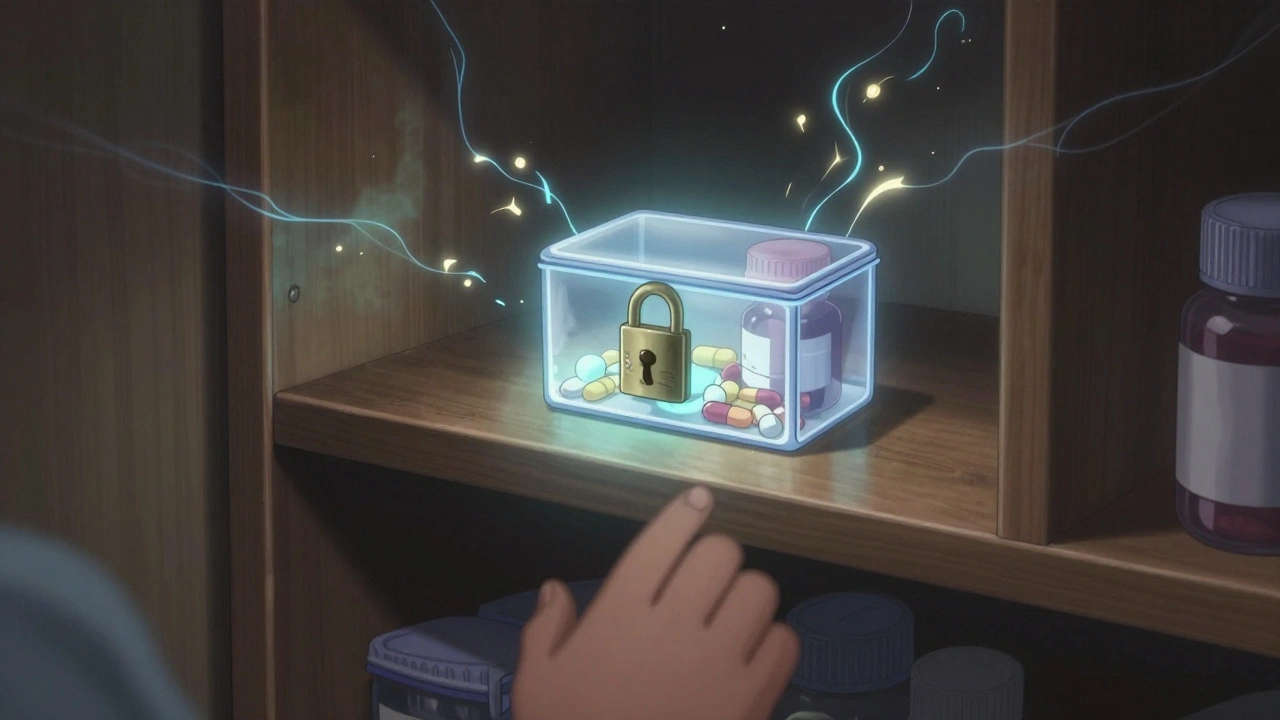
There’s also the risk of mixing opioids with other meds. Alcohol, benzodiazepines, sleep aids, and even some cold medicines can turn a safe dose into a deadly one. You don’t need to be a pharmacist to know this—just read the label and ask your pharmacist. And if you’re storing opioids at home, keep them locked up. Kids, teens, and visitors can accidentally—or intentionally—take them. A single pill can be fatal to someone who hasn’t built tolerance.
What you’ll find in the posts below isn’t just a list of facts. It’s real, practical guidance from people who’ve been through it: how to spot the early signs of misuse, what to do if someone stops breathing, why some people are more at risk than others, and how to talk to your doctor without feeling judged. These aren’t theoretical warnings. They’re stories from patients, caregivers, and clinicians who’ve seen the cost of ignoring opioid safety—and how to prevent it.