When you find out you're pregnant, your body changes in ways you can't always see. One of the most important but often overlooked shifts happens in your thyroid. If you're already taking thyroid medication-usually levothyroxine-your dose likely needs to go up. Not tomorrow. Not next month. Now.
Why Thyroid Medication Changes in Pregnancy
Your thyroid makes hormones that control metabolism, energy, and, most critically for your baby, brain development. Before pregnancy, your body runs on a steady supply. But as soon as you conceive, your baby starts relying on your thyroid hormones for the first 10 to 12 weeks. During that time, your baby can't make its own. If your hormone levels drop even slightly, it can affect how your child’s brain develops. Research shows that untreated or poorly managed hypothyroidism during pregnancy increases the risk of miscarriage by up to 60% and lowers a child’s IQ by 7 to 10 points on average. That’s not a small difference-it’s the gap between average and above-average cognitive performance. The good news? Getting your dose right can prevent almost all of these risks.How Much More Medication Do You Need?
Most women with pre-existing hypothyroidism need 20% to 30% more levothyroxine as soon as they confirm pregnancy. That might sound like a lot, but it’s not guesswork. It’s science. A 2021 NIH study of 280 pregnant women found their average daily dose jumped from 85.7 mcg before pregnancy to 100.0 mcg in the first trimester. That’s a 14.3 mcg increase-roughly one extra tablet every few days. For some, that means adding a 12.5 mcg or 25 mcg pill. For others, it’s doubling their weekly dose on two extra days. Guidelines vary slightly. The American Thyroid Association says to increase your dose by 20-30% immediately after a positive pregnancy test. The American College of Obstetricians and Gynecologists (ACOG) recommends a bigger jump: a 50 mcg increase right away for women already on medication. Why the difference? Because some women need more, and some need less. The key is not to wait. If you’re newly diagnosed during pregnancy, your starting dose depends on your TSH level:- If your TSH is 10 mIU/L or higher: Start at 1.6 mcg per kg of body weight per day.
- If your TSH is under 10 mIU/L: Start at 1.0 mcg per kg per day.
When to Adjust Your Dose
Don’t wait for your first prenatal visit. Don’t wait until you feel tired or cold. Don’t wait for your doctor to bring it up. The moment you know you’re pregnant, increase your dose. Why? Because your baby’s brain is already developing. By week 6, your baby’s thyroid gland is forming, but it still can’t make hormones. Until week 12, it’s all on you. Delaying a dose increase-even by a few weeks-can mean missing a critical window for neurodevelopment. A 2021 study found that women who had their levothyroxine dose adjusted within four weeks of confirmation had 23% fewer preterm births than those who waited longer. That’s not just a statistic. It’s a real outcome: a baby born at 39 weeks instead of 35, a baby who doesn’t spend time in the NICU, a baby who starts life with fewer risks.How to Take Your Medication Correctly
Taking levothyroxine isn’t just about the dose-it’s about how you take it. If you’re not doing it right, your body won’t absorb enough.- Take it on an empty stomach, at least 30 to 60 minutes before eating.
- Avoid calcium, iron, or prenatal vitamins within 4 hours. These minerals bind to the medication and block absorption by up to 50%.
- Don’t switch brands unless your doctor says so. Synthroid, Tirosint, and generic levothyroxine aren’t always interchangeable. Even small differences in fillers can affect how your body uses the drug.
- If you miss a dose, take it as soon as you remember. If it’s almost time for your next dose, skip the missed one. Don’t double up.

Monitoring TSH: The Gold Standard
You can’t guess if your dose is right. You can’t feel it. You need a blood test. The American Thyroid Association recommends checking your TSH:- Within 4 weeks of any dose change
- Every 4 weeks until your levels stabilize
- At least once per trimester after that
- First trimester: ≤2.5 mIU/L
- Second trimester: ≤3.0 mIU/L
- Third trimester: ≤3.0 mIU/L
What If You’re Not on Medication Yet?
Not everyone knows they have hypothyroidism before pregnancy. Some women are diagnosed during prenatal screening. If your TSH is above 4.0 mIU/L, you should start levothyroxine immediately. Even if you have no symptoms. The 2023 ATA guidelines now recommend universal TSH screening for all pregnant women in the first trimester. That’s a big shift. Just five years ago, only high-risk women were tested. Now, because of the evidence linking low thyroid hormone to poor outcomes, screening is becoming standard. If you’re planning pregnancy and have a history of thyroid disease, autoimmune conditions, or a family history of thyroid disorders, get your TSH checked before you conceive. Don’t wait.Real Stories, Real Consequences
One patient on Reddit wrote: “My OB said, ‘Wait and see.’ I waited eight weeks. My TSH was 5.8. I was terrified my baby wouldn’t be okay.” She ended up increasing her dose by 50 mcg, then another 25 mcg. Her baby was born healthy-but she spent months in anxiety. Another woman, on HealthUnlocked, said: “I increased my dose the day I got a positive test. My TSH stayed under 1.5 the whole pregnancy. My daughter is now 18 months and hitting every milestone early.” The difference? Timing. Action. Advocacy.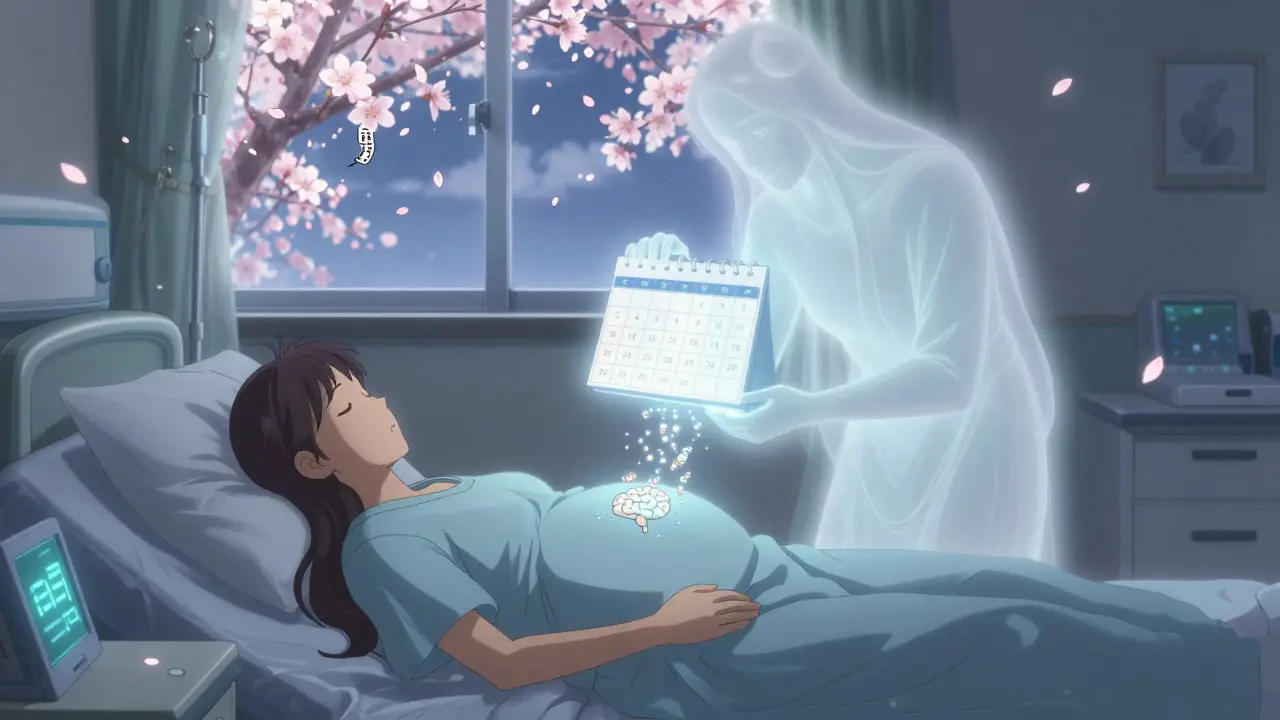



Selina Warren
January 18, 2026 AT 11:27Okay, let’s cut the fluff-this is life-or-death stuff. I had my dose bumped the second I saw that positive line. My OB shrugged and said, ‘We’ll check in next month.’ I didn’t wait. I called my endo myself. TSH was 4.1 at 5 weeks. By week 8, I was on 112 mcg. Baby’s now 14 months, walking, talking, crushing milestones. If you’re waiting for permission-you’re already late.
Robert Davis
January 19, 2026 AT 00:33Interesting. I wonder if the 20-30% increase is based on population averages or individual metabolic rates. I’ve read studies where weight-based dosing shows more precision, especially in obese patients. The guidelines seem… oversimplified.
Eric Gebeke
January 19, 2026 AT 01:16So let me get this straight-you’re telling women to just up their meds like they’re coffee? No testing? No caution? What if you overshoot and get hyperthyroid? Then you’re risking preterm labor, fetal tachycardia, even stillbirth. This isn’t ‘just take more pills’-it’s medical malpractice waiting to happen if you don’t monitor.
Chuck Dickson
January 19, 2026 AT 17:19Hey, if you’re reading this and you’re pregnant and on levothyroxine-stop scrolling. Go check your last TSH. If it’s been longer than 6 weeks, call your doctor. If they don’t know the guidelines, print this out and hand it to them. You’re not being annoying-you’re protecting your baby’s future. I’ve seen too many women panic because they were told to ‘wait and see.’ Don’t be one of them. You’ve got this.
rachel bellet
January 21, 2026 AT 09:39While the 20-30% increase is statistically significant in cohort studies, the effect size on neurocognitive outcomes remains confounded by maternal BMI, iodine status, and TPOAb positivity. The ACOG recommendation of a 50 mcg bolus lacks stratification for baseline TSH, potentially inducing iatrogenic hyperthyroidism in low-demand phenotypes. The evidence base is robust but not granular enough for precision dosing.
Pat Dean
January 22, 2026 AT 09:29Why are we letting Big Pharma dictate prenatal care? Levothyroxine is cheap. Why do they push brand names? Why do hospitals use Epic alerts but not mandate testing? This is profit-driven medicine. Wake up.
Joni O
January 24, 2026 AT 05:46i just found out i’m preggo last week and i’ve been on synthroid for 5 years… i was so scared to up my dose cause i didn’t wanna mess up. but after reading this i called my dr today and they said ‘good job for asking’ and bumped me up right away. tsh was 3.8 at 6w. now i’m on 100mcg. thank you for this. i feel less alone.
Max Sinclair
January 26, 2026 AT 03:46Appreciate the clarity here. I’ve been a nurse for 12 years and I’ve seen too many patients get dismissed because ‘they don’t feel sick.’ Thyroid issues don’t always show symptoms until it’s too late. This post should be required reading for every OB-GYN and every woman planning a pregnancy.
christian Espinola
January 26, 2026 AT 19:47Who funded this study? Big Pharma? The thyroid industry makes billions. You think they want you to just take a pill and call it a day? What about natural alternatives? Selenium? Ashwagandha? Why isn’t anyone talking about the root cause?
Dayanara Villafuerte
January 28, 2026 AT 19:14👏👏👏 YES. This. I’m a thyroid warrior mom. Took 12.5 mcg extra every Tue/Thu. No calcium within 4 hours. Got my TSH down to 1.2 at 10 weeks. Baby’s 2 now and reading books at 18 months. 🤓📚 Don’t sleep on this. Your kid’s IQ isn’t a gamble. 🧠💪
kenneth pillet
January 30, 2026 AT 07:15my doc said wait till 8 weeks. i did. tsh was 5.1. i cried. increased dose by 50 mcg. now its 100. next test in 2 weeks. hope its ok
Kristin Dailey
January 31, 2026 AT 07:08Stop waiting. Increase now. Test in 4 weeks. That’s it.
Jay Clarke
February 1, 2026 AT 03:18They told me to wait. I didn’t. I took the 25 mcg extra on day one. My doctor called me a ‘hypochondriac.’ My baby is now a healthy 3-year-old who speaks three languages. Don’t let anyone make you feel crazy for protecting your child. You’re not being dramatic-you’re being a parent.
Jake Moore
February 2, 2026 AT 04:25One thing no one mentions: if you’re on generic levothyroxine, stick to the same batch. I switched brands after my insurance changed and my TSH spiked from 1.8 to 4.3 in 3 weeks. Same dose. Different filler. My endo said it’s ‘not supposed to matter.’ It did. Don’t assume all levothyroxine is equal.
Praseetha Pn
February 3, 2026 AT 03:25HAHAHAHA you think this is the only thing they hide? Wait till you find out about the fluoride in water and how it blocks iodine uptake. And the soy in baby formula? And the glyphosate in your gluten-free oats? Thyroid is the canary in the coal mine. This is just step one. The system is rigged. I’ve been tracking my TSH since 2018. I know what they don’t want you to know.