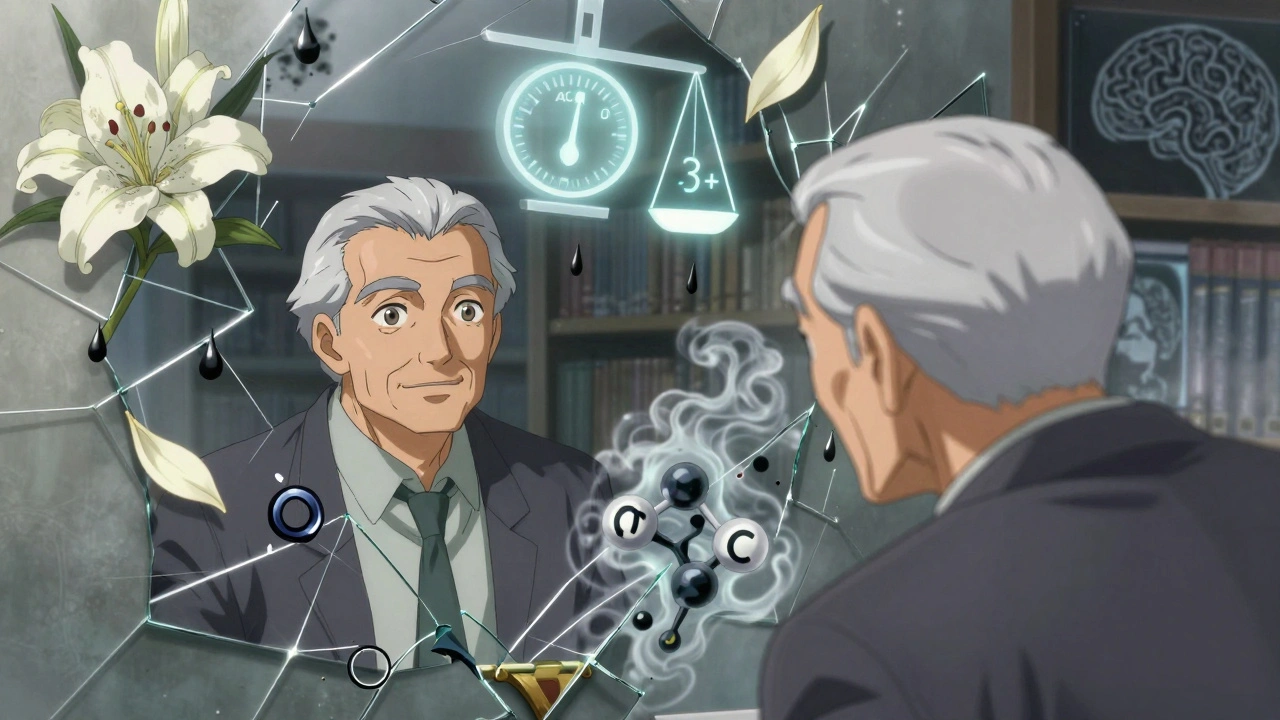
Anticholinergic Burden Calculator
This calculator helps you understand your anticholinergic burden from medications. A score of 3 or higher indicates increased dementia risk. The ACB scale rates medications from 1 (low) to 3 (high) based on their brain impact.
No medications selected yet
Your Anticholinergic Burden Score: 0
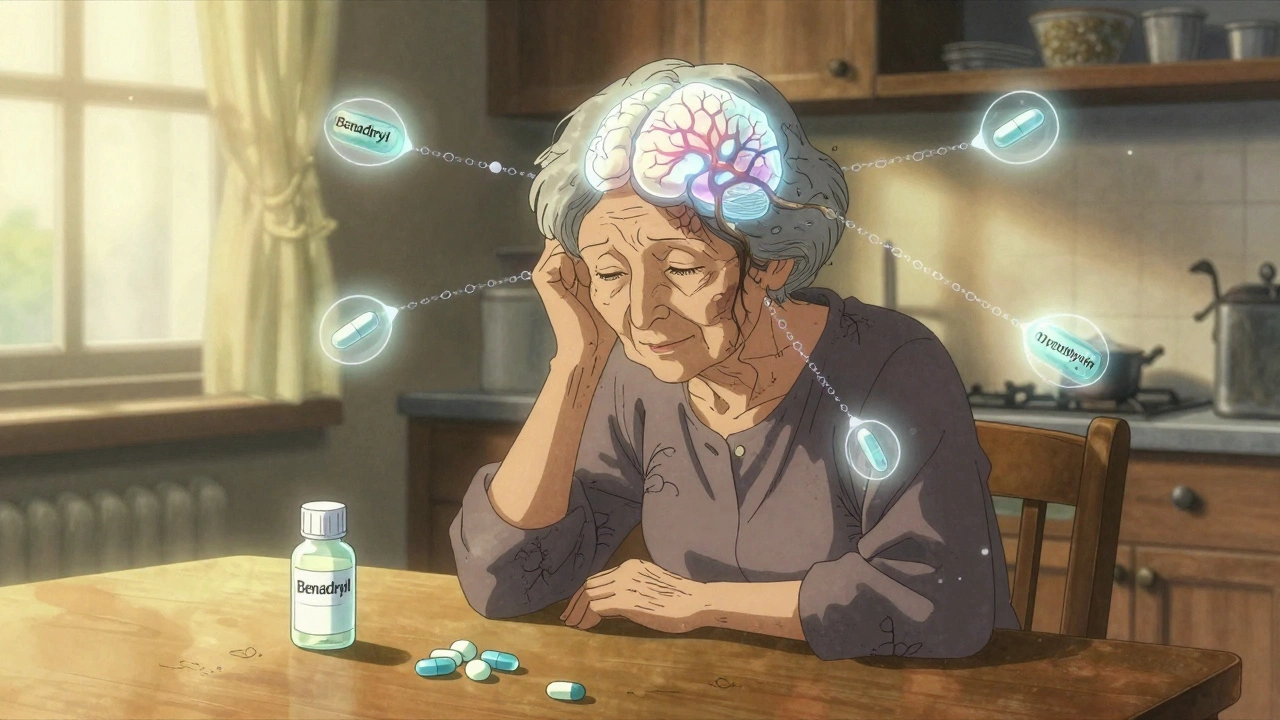
Many older adults take medications for common issues like allergies, bladder problems, depression, or insomnia without realizing they might be slowly harming their brain. Drugs like Benadryl, oxybutynin, and amitriptyline are everywhere - in medicine cabinets, pharmacy shelves, and prescriptions. But growing evidence shows these anticholinergic medications may be linked to long-term memory loss and a higher chance of developing dementia. This isn’t just a theoretical concern. It’s happening right now, in homes across the country, often unnoticed until it’s too late.
What Are Anticholinergic Medications?
Anticholinergic drugs work by blocking acetylcholine, a chemical in your brain and body that helps nerves communicate. This can be helpful for stopping muscle spasms, reducing saliva, or calming an overactive bladder. But when this blockage happens in the brain, it slows down thinking, memory, and attention. Over time, that slowdown can turn into something more serious.
There are about 100 common medications with anticholinergic effects. They fall into several categories:
- Antihistamines - like diphenhydramine (Benadryl), chlorpheniramine (Chlor-Trimeton)
- Bladder medications - oxybutynin (Ditropan), tolterodine (Detrol), solifenacin (Vesicare)
- Antidepressants - amitriptyline (Elavil), doxepin (Sinequan), imipramine (Tofranil)
- Antipsychotics - quetiapine (Seroquel), olanzapine (Zyprexa)
- Parkinson’s drugs - trihexyphenidyl (Artane), benztropine (Cogentin)
Not all of these are prescription-only. Many are sold over the counter. That’s part of the problem. People don’t think of Benadryl as a brain-altering drug. But it is - especially when taken regularly for months or years.
The Link Between Anticholinergics and Dementia
Multiple large studies have now shown a clear connection. One study tracking over 3,400 adults for more than 10 years found that those who took strong anticholinergic drugs for three years or more had a 50% higher risk of developing dementia compared to those who didn’t take them. That’s not a small increase - it’s a major red flag.
Brain scans from these studies show something even more concerning. People on these medications had faster shrinkage in the hippocampus - the part of the brain that stores memories. They also showed lower glucose use in brain areas linked to thinking and attention. In simpler terms: their brains were working less efficiently, and the damage was visible on scans.
It’s not just about taking one pill. The risk builds up over time. This is called anticholinergic burden. It’s measured using tools like the Anticholinergic Cognitive Burden (ACB) scale. A score of 3 or higher means you’re on a drug or combination of drugs with strong anticholinergic effects. That’s where the risk spikes.
Some Drugs Are Riskier Than Others
Not all anticholinergics are created equal. Some cross the blood-brain barrier easily and hit the brain hard. Others barely make it past. That’s why two people taking different bladder meds might have very different outcomes.
For example:
- Oxybutynin - high risk. Linked to a 23% higher dementia risk.
- Solifenacin - also high risk. 20% increased risk.
- Trospium - no significant link. A safer option.
Same condition. Different drugs. Big difference in risk.
Antidepressants like amitriptyline carry the highest dementia risk among all anticholinergics - 29% higher than non-users. That’s worse than many blood pressure or cholesterol meds. And yet, many doctors still prescribe them to older adults because they’re cheap and effective for nerve pain or depression.
Who’s Most at Risk?
It’s not just age. It’s exposure. People over 65 are more vulnerable because their brains are already dealing with natural aging changes. But even people in their 50s aren’t safe. The damage starts long before dementia symptoms show up.
Those with a family history of Alzheimer’s, especially those carrying the APOE-ε4 gene, are at even higher risk. Studies are now tracking these individuals to see if stopping anticholinergics early can delay or even prevent dementia.
Women are also more likely to be prescribed these drugs - especially for overactive bladder or chronic pain. That means they may be exposed to higher cumulative doses over time.
What Patients Don’t Know - And What Doctors Might Not Tell Them
Here’s the uncomfortable truth: most people on these meds have no idea they’re taking something that could hurt their brain. A 2021 survey found that only 37% of primary care doctors routinely check for anticholinergic burden in patients over 65. Even though 89% of them say they know it’s a risk, they don’t act on it.
Patients often don’t connect their brain fog, memory lapses, or trouble concentrating to their meds. They think it’s just getting older. Or they’re told, “It’s just a side effect - it’ll go away.” But research shows it doesn’t always go away. One Reddit user shared that her mother’s memory score dropped from 28 to 22 over three years on amitriptyline. Even after stopping, it never fully recovered.
On Drugs.com, 68% of people say oxybutynin works great for bladder control. Only 22% mention cognitive side effects. That gap between experience and awareness is huge. And it’s dangerous.
What Can You Do?
You don’t have to live with brain fog or fear dementia. There are safer options - and steps you can take right now.
1. Review your meds
Make a list of every pill, patch, or liquid you take - including OTC drugs and supplements. Bring it to your doctor or pharmacist. Ask: “Is this anticholinergic? What’s the ACB score?”
2. Ask for alternatives
- For overactive bladder: Ask about mirabegron (Myrbetriq) instead of oxybutynin. It’s just as effective but has zero anticholinergic effect.
- For depression or nerve pain: SSRIs like sertraline or escitalopram are safer than tricyclics like amitriptyline.
- For insomnia: Try sleep hygiene, CBT-I (cognitive behavioral therapy for insomnia), or melatonin instead of diphenhydramine.
3. Don’t stop cold turkey
Some of these drugs cause withdrawal symptoms if stopped suddenly. Muscle cramps, nausea, or even rebound bladder problems can happen. Work with your doctor to taper off slowly - usually over 4 to 8 weeks.
4. Track your brain health
Simple memory tests, like recalling three words after five minutes, can be done at home. If you notice a change - forgetting names, missing appointments, struggling with directions - talk to your doctor. Don’t wait.
The Bigger Picture
Reducing anticholinergic use isn’t just about individual health. It’s a public health opportunity. The Alzheimer’s Association estimates that cutting out these drugs could prevent up to 15% of dementia cases each year - that’s over half a million people worldwide.
Organizations like the American Geriatrics Society are pushing for change. Their Beers Criteria now strongly advise against using strong anticholinergics in older adults. Electronic health records like Epic now include built-in anticholinergic burden calculators to alert doctors before they prescribe.
But progress is slow. Only 42% of drug leaflets in Europe include warnings about cognitive risks - even though regulations require it. In the U.S., the FDA added stronger warnings to 14 anticholinergic drugs in 2020. But patients still pick them off the shelf without reading the fine print.
What’s Next?
Research is moving fast. The PREPARE trial, launched in 2023, is following 3,000 people with a genetic risk for Alzheimer’s to see if stopping anticholinergics slows cognitive decline. Early results are expected by 2028.
Meanwhile, pharmaceutical companies are developing new drugs that treat the same conditions without crossing into the brain. Seven new bladder medications and three new antidepressants are in late-stage trials - all designed to avoid anticholinergic effects.
Change is coming. But it won’t happen unless patients and doctors work together. You have the power to ask questions. To push for safer options. To protect your brain - before it’s too late.


John Fred
December 12, 2025 AT 22:01Bro, I just checked my meds - Benadryl for sleep, oxybutynin for bladder, and amitriptyline for nerve pain 😱 ACB score of 4? That’s like a dementia triple threat. I’m scheduling a med review this week. Thanks for the wake-up call 🙏🧠
Harriet Wollaston
December 14, 2025 AT 04:03I’m so glad someone finally said this. My mom was on amitriptyline for years - she thought her forgetfulness was just ‘getting old.’ When she switched to sertraline, it was like a fog lifted. She remembered my birthday again. Small wins matter. 💕
sharon soila
December 14, 2025 AT 19:00Knowledge is power. But power without action is just noise. You have a right to your brain. You have a right to clarity. You have a right to live without silent erosion. Start with the list. Talk to your pharmacist. Ask for alternatives. This isn’t fear. It’s responsibility. And responsibility is the highest form of love - for yourself.
nina nakamura
December 15, 2025 AT 12:44Hamza Laassili
December 17, 2025 AT 10:50Rawlson King
December 17, 2025 AT 21:38It’s not the drugs. It’s the lack of discipline. People take these because they don’t want to do pelvic floor exercises or sleep hygiene. The real issue is laziness disguised as medical need. Stop looking for easy fixes - your brain isn’t a vending machine.
Constantine Vigderman
December 18, 2025 AT 04:53OMG I just looked up my meds - I’ve been taking diphenhydramine for YEARS 😳 I thought it was just a sleepy pill! I’m switching to melatonin and CBT-I right now. Also, my doc never even mentioned ACB score… why is this not standard?? 🤯 #BrainHealth #MedicationAwareness
Cole Newman
December 19, 2025 AT 08:32Wait so you’re telling me my grandma’s memory loss is from her allergy pills? She’s been on Benadryl since 2010. I’m calling her doctor right now. She thinks it’s normal to be confused. I didn’t realize it was the meds. Thanks for making me feel guilty… but also motivated.
Bruno Janssen
December 20, 2025 AT 16:33I’ve been on oxybutynin for 7 years. I didn’t realize I was forgetting my grandkids’ names because of it. I just thought I was… tired. I stopped last month. Still foggy. Still scared. I hope it gets better. I miss who I was.
Deborah Andrich
December 21, 2025 AT 02:08Tommy Watson
December 21, 2025 AT 07:26So what? My aunt took 10 different anticholinergics and lived to 92. She still remembers every detail of her wedding. Maybe it’s not the meds - maybe it’s just genetics. Stop scaring people with stats. Some of us are fine. And some of us don’t want to live in fear.