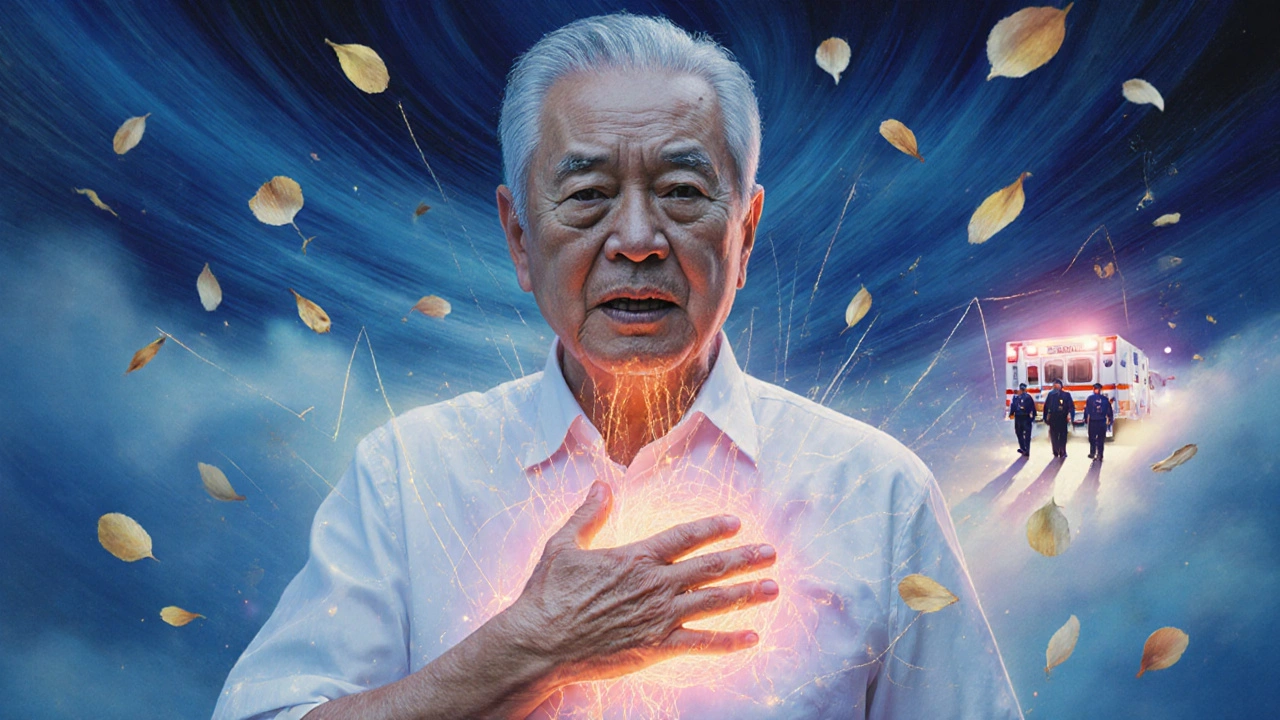
When your chest hurts, it’s easy to panic. Is it heartburn? A pulled muscle? Or something life-threatening? The truth is, chest pain isn’t always a heart attack-but it can be. Knowing when to call 9-1-1 instead of waiting it out or driving yourself to the hospital can save your life.
What Counts as Chest Pain?
Chest pain isn’t just a sharp stab or squeezing feeling in the center of your chest. It can show up as pressure, tightness, burning, or even just a strange discomfort. And it doesn’t always stay in your chest. Many people feel it in their jaw, neck, back, shoulders, or arms. Some don’t feel pain at all-they just feel dizzy, short of breath, nauseous, or suddenly exhausted. These are called anginal equivalents, and they’re just as important as classic chest pain when it comes to heart problems.When to Go to the Emergency Department
You don’t need to be sure it’s a heart attack to go to the ER. If you’re unsure, err on the side of caution. Here’s when you should call emergency services right away:- Pressure, squeezing, or heaviness in your chest that lasts more than a few minutes-or comes and goes
- Pain that spreads to your arm, neck, jaw, or back
- Shortness of breath with chest discomfort
- Sudden cold sweat, nausea, or vomiting
- Feeling lightheaded, faint, or like you’re going to pass out
- Unexplained fatigue that comes out of nowhere, especially if you’re over 50 or have risk factors like high blood pressure or diabetes
These symptoms don’t have to be dramatic. A 68-year-old woman might not feel chest pain at all-she might just feel like she’s been hit by a truck and can’t catch her breath. That’s still a red flag.
Why You Shouldn’t Drive Yourself
Driving yourself to the hospital sounds practical, but it’s risky. Studies show that people who drive themselves to the ER have a 25-30% higher chance of having a bad outcome during transport. Why? Because if your heart stops or you go into a dangerous rhythm, no one’s there to help. Emergency Medical Services (EMS) teams are trained to monitor your heart, give oxygen, and even start life-saving treatments before you even reach the hospital. They can also send your ECG results ahead, so the ER team is ready the moment you walk in.The First 10 Minutes Matter
Once you arrive at the ER, time is everything. The first thing they’ll do is get a 12-lead electrocardiogram (ECG)-and they’re required to do it within 10 minutes of your arrival. This simple test checks your heart’s electrical activity. It can show if you’re having a heart attack right now, especially if there’s a pattern called ST-elevation (STEMI). If you have that, they’ll rush you to the cath lab for a procedure to open your blocked artery. The goal? Get the balloon in and the artery open within 90 minutes of your arrival.But not all heart attacks show up on the first ECG. That’s why doctors often repeat the test every 15-30 minutes if your symptoms are still there. A normal ECG doesn’t rule out a heart attack-it just means you need more tests.

Troponin: The Blood Test That Tells the Truth
The next key test is a blood test for cardiac troponin. This protein leaks into your bloodstream when heart muscle is damaged. Modern hospitals use high-sensitivity troponin assays, which can detect tiny amounts of damage. Most patients get two tests: one when they arrive, and another one or two hours later.If the troponin levels stay low and don’t rise over time, and your ECG looks normal, there’s a 90% chance you’re not having a heart attack. In fact, about 70-80% of chest pain patients in the ER are ruled out for a heart attack within just two hours using this method. That means you might be sent home with a follow-up appointment instead of a hospital stay.
What If It’s Not a Heart Attack?
Not every chest pain is cardiac. Other common causes include:- Acid reflux (heartburn)
- Muscle strain or rib injury
- Anxiety or panic attacks
- Pulmonary embolism (blood clot in the lung)
- Pericarditis (inflammation around the heart)
Doctors use more than just symptoms to tell the difference. They look at your age, risk factors (smoking, high cholesterol, diabetes, family history), and physical exam signs. If you’re young, healthy, and the pain changes with movement or breathing, it’s less likely to be heart-related. But if you’re over 50, have high blood pressure, and your pain comes with sweating and nausea? That’s a red flag.
The HEART Score: A Simple Tool for Risk
Many ERs use a tool called the HEART score to help decide how worried they should be. It looks at five things:- History: How much does your pain match typical heart attack symptoms?
- ECG: Are there any abnormal patterns?
- Age: Are you over 65?
- Risk factors: Do you smoke, have diabetes, or high cholesterol?
- Troponin: What’s the level in your blood?
Each item gets a score of 0, 1, or 2. Add them up:
- 0-3 = Low risk (you can likely go home with follow-up)
- 4-6 = Intermediate risk (you’ll need more testing, like a stress test or CT scan)
- 7-10 = High risk (you’re going straight to the cath lab)
This isn’t perfect-but it helps doctors make faster, more consistent decisions.

What Happens After the ER?
If you’re ruled out for a heart attack, you might still need follow-up. Some people have INOCA-ischemia with no obstructive coronary artery disease. That means their heart isn’t getting enough blood, but their arteries aren’t clogged. It’s more common in women and people with diabetes. These cases need specialized testing like coronary CT angiography or cardiac MRI.Even if you’re low risk, your doctor will likely ask you to see a cardiologist within a week. They’ll check for underlying issues like high cholesterol, high blood pressure, or early signs of artery disease. Preventing the next episode is just as important as treating the current one.
What to Do Before You Go
If you’re worried about chest pain:- Don’t wait. Don’t try to tough it out.
- Call 9-1-1. Don’t drive yourself.
- Chew one adult aspirin (325 mg) if you’re not allergic and it’s safe to do so. Aspirin can help reduce clotting while you wait for help.
- Stay calm. Panic raises your heart rate and can make things worse.
- Have your medications, allergies, and medical history ready to tell the paramedics.
What You Should Know About New Tech
By 2025, most U.S. hospitals will use AI to help read ECGs. These systems can spot subtle changes that even experienced doctors might miss-like early signs of a heart attack hours before symptoms get worse. That means faster, more accurate decisions. But the human touch still matters. The best outcomes come when technology and clinical judgment work together.Final Thought: Better Safe Than Sorry
Chest pain is one of the most common reasons people go to the ER. And while only 10-15% of those cases turn out to be heart attacks, that’s still thousands of lives saved every year because someone didn’t ignore the warning.You don’t need to be an expert to know when something’s wrong. If your body feels like it’s screaming for help, listen to it. Call 9-1-1. Let the professionals sort it out. The cost of waiting could be your life-or the life of someone you love.
Can chest pain be caused by something other than a heart attack?
Yes. Many non-heart conditions cause chest pain, including acid reflux, muscle strain, anxiety, lung clots, or inflammation around the heart. But because it’s hard to tell the difference without tests, any new or unexplained chest pain should be evaluated in an emergency setting to rule out life-threatening causes.
Is it safe to wait and see if chest pain goes away?
No. If chest pain is new, persistent, or worsening, waiting can be dangerous. Heart attacks can progress quickly, and early treatment saves heart muscle and lives. Even if it turns out to be something minor, it’s better to be checked than to risk a delay that could cost you your life.
Do I need an ECG if I’m young and healthy?
Yes. Heart attacks can happen at any age, especially with risk factors like smoking, obesity, or family history. The ECG is quick, painless, and gives critical information in minutes. Even young people with no known conditions can have heart problems-especially if symptoms are present.
Can I use a home ECG device like Apple Watch to check for a heart attack?
Home devices can detect irregular heart rhythms like atrial fibrillation, but they cannot reliably diagnose a heart attack. They don’t capture the full 12-lead ECG needed to spot ST-elevation or other key signs. If you have chest pain, call emergency services-not your smartwatch.
Why do I need two troponin tests?
Troponin levels rise slowly after heart damage. One test might show normal levels even if a heart attack is starting. A second test 1-2 hours later shows whether levels are increasing-which confirms heart muscle injury. This two-step process is what makes modern chest pain evaluation so accurate.
What if I have chest pain but no risk factors?
Risk factors increase your chances, but they don’t guarantee safety. About 1 in 5 heart attacks happen in people with no known risk factors. If you have symptoms like chest pressure, sweating, nausea, or shortness of breath, don’t rely on your risk profile to decide whether to go to the ER. Symptoms matter more than statistics.
Can stress or anxiety cause chest pain that feels like a heart attack?
Yes. Panic attacks can cause chest tightness, rapid heartbeat, and shortness of breath that mimic a heart attack. But the key difference is timing and triggers. Anxiety-related pain often comes with hyperventilation, tingling in hands or face, and a sense of dread. Still, if you’re unsure, it’s safer to get checked. Emergency staff can quickly tell the difference with tests.
Should I take aspirin before calling 9-1-1?
If you’re not allergic to aspirin and don’t have a bleeding disorder, chewing one adult aspirin (325 mg) while waiting for EMS can help reduce clotting. But don’t delay calling 9-1-1 to find aspirin. Calling first is more important than taking it.
What if I’m not sure whether it’s serious?
If you’re unsure, assume it’s serious. Emergency departments are designed to handle uncertainty. It’s better to be evaluated and told it’s nothing than to ignore a warning sign. Paramedics and ER staff see hundreds of chest pain cases every year-they’re trained to sort through the noise.
How long does chest pain evaluation take in the ER?
For low-risk patients, evaluation can be complete in 1-2 hours. For those with clear signs of a heart attack, treatment starts immediately. Intermediate-risk cases may take longer-up to 6-8 hours-for additional tests. The goal is to get you the right answer as fast as possible, without unnecessary delays.
Remember: Your heart doesn’t always warn you with a siren. Sometimes, it whispers. Listen before it’s too late.


Brandy Walley
November 21, 2025 AT 17:49shreyas yashas
November 23, 2025 AT 14:02Ragini Sharma
November 24, 2025 AT 22:05Linda Rosie
November 25, 2025 AT 18:42Lisa Lee
November 25, 2025 AT 21:16Jennifer Shannon
November 27, 2025 AT 02:48Suzan Wanjiru
November 27, 2025 AT 08:11Kezia Katherine Lewis
November 28, 2025 AT 15:16