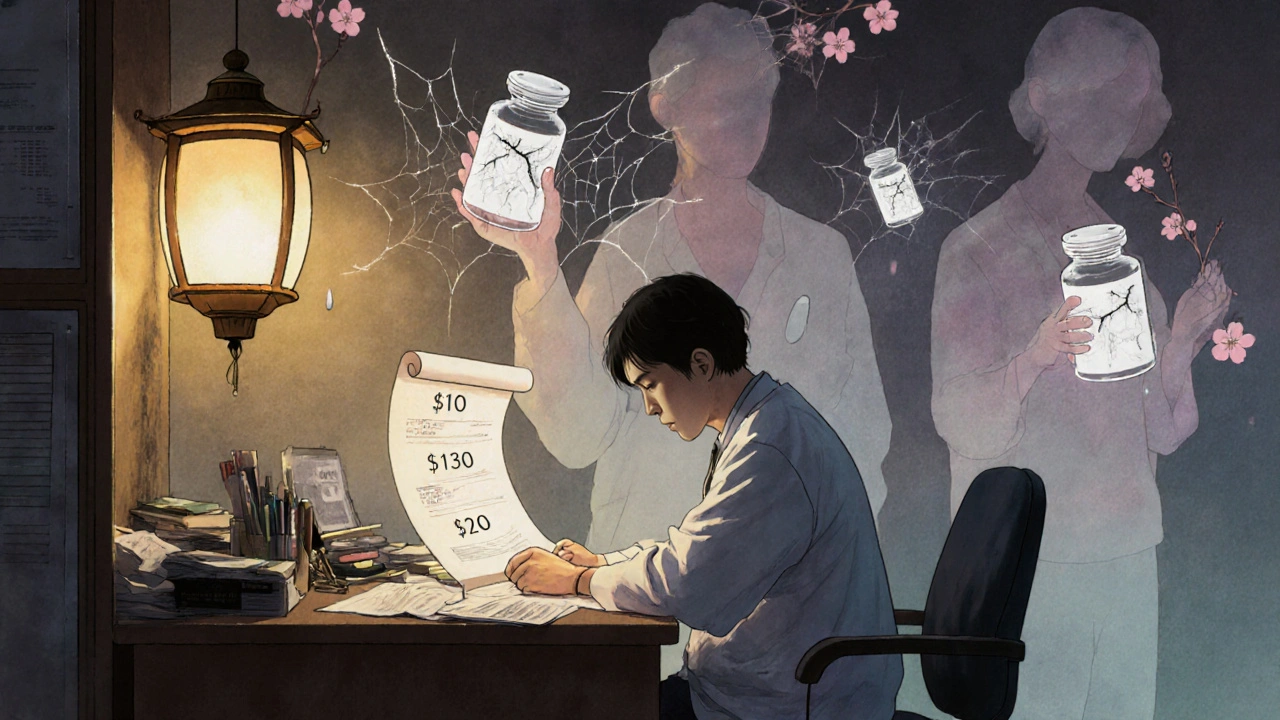
Imagine you’re a doctor. Your patient walks in with chest pain. You write a prescription for a statin. You don’t check the price. You assume it’s $10 a month. It’s actually $320. The patient skips doses. Three months later, they’re back in the ER. This isn’t hypothetical. It happens every day.
Doctors are guessing at drug prices - and getting it wrong
A 2007 review of 29 studies found doctors consistently misjudge drug costs. They overestimate cheap drugs by 31%. They underestimate expensive ones by 74%. That’s not a small mistake. It’s a systemic blind spot. When a doctor prescribes a $15 generic, they think it’s $20. When they pick a $500 brand-name drug, they think it’s $130. That’s not just inaccurate - it’s dangerous. The numbers don’t lie. One study of 254 medical students and doctors found only 5.4% of generic drug costs were estimated within 25% of the real price. For brand-name drugs, it was 13.7%. That means over 85% of the time, clinicians were off by more than a quarter of the actual cost. And here’s the kicker: they were more confident in their wrong answers than in the ones they got right.Why does this gap exist?
Medical school doesn’t teach drug pricing. Not really. A 2021 study found 56% of U.S. medical schools have no formal curriculum on how drugs are priced. Students learn about mechanisms of action, side effects, dosing - but not about the $621 billion U.S. prescription market. They graduate thinking a drug’s price reflects R&D costs. It doesn’t. Only 44% of students know that drug prices have almost nothing to do with research spending. Most pricing is set by manufacturers, insurers, and pharmacy benefit managers - none of which are discussed in lecture halls. Clinicians also don’t have access to real-time data. A 2007 survey showed 92% of doctors wanted cost information at the point of care - but couldn’t find it. Today, that’s still true for most. Even when EHRs show a drug’s list price, it doesn’t tell you what the patient will actually pay. A $200 drug might be $5 with insurance. Or $400 if they’re on a high-deductible plan. Or $15 at Walmart. No single source gives you the full picture.The real cost isn’t just money - it’s health
When patients can’t afford their meds, they skip doses. Cut pills in half. Stop taking them altogether. The Kaiser Family Foundation found 28% of U.S. adults have skipped medication due to cost. That’s 1 in 4 people. And it’s not just low-income patients. Even people with insurance are cutting corners. A 2023 KFF report showed 82% of adults think drug prices are unreasonable. The consequences are measurable. Patients who don’t take their statins because of cost have a 30% higher risk of heart attack. Those who skip insulin face diabetic ketoacidosis. Those who stop blood pressure meds risk stroke. These aren’t abstract risks. They’re emergency room visits, hospitalizations, and early deaths - all preventable if the doctor knew the price and chose an affordable alternative.
Technology can help - but it’s not perfect
Some hospitals are trying to fix this. UCHealth, Harvard, and others have built real-time benefit tools (RTBTs) that pop up in EHRs when a doctor writes a prescription. These tools show the patient’s out-of-pocket cost based on their insurance. In one study, one in eight doctors changed their prescription after seeing the alert. When potential savings were over $20, that number jumped to one in six. But here’s the problem: these tools are inaccurate. A resident on Reddit wrote: “Our Epic system shows insurer pricing but doesn’t account for my patient’s specific copay. Half the time, it’s wrong.” That’s because drug pricing is a maze. The same drug can cost $15 at one pharmacy, $320 at another. Insurers negotiate different rates. Pharmacy networks change. Prior authorizations vary. No system can keep up perfectly. And adoption is low. Only 37% of U.S. health systems have RTBTs installed as of late 2024. Many hospitals say it’s too expensive - UCHealth spent $2.3 million and 18 months building theirs. Others say clinicians don’t use them. But data shows the opposite: doctors under 40 adopt these tools at a 78% rate. Those over 55? Only 52%. The gap isn’t resistance - it’s access.What’s changing - and what’s not
The Inflation Reduction Act of 2022 gave Medicare the power to negotiate drug prices. That’s a big deal. It’s the first time the government has directly intervened to cap prices. And it’s popular. 83% of Democrats and 76% of Republicans support it. That’s rare bipartisan agreement. Meanwhile, drug manufacturers keep raising prices without clinical justification. In 2023, five major drugs - including Humira - got price hikes of 4.7% or more, even though no new benefits were added. The Institute for Clinical and Economic Review called it “medically unnecessary.” But without price transparency, doctors can’t push back. The American Medical Association and American College of Physicians have both declared cost-conscious prescribing a professional priority since 2015. Yet most doctors still don’t know how to do it. They’re not lazy. They’re not uncaring. They’re just not trained.


Evelyn Shaller-Auslander
November 29, 2025 AT 04:35this is so real i had a friend skip her blood pressure meds for months cuz she thought the copay was $5 but it was $80... she ended up in the hospital. doctors just dont know.
no one talks about this.
Gus Fosarolli
November 29, 2025 AT 09:15so let me get this straight - we train doctors to memorize 47 different beta-blockers but not how much a pill costs? that’s like teaching chefs to identify 20 types of salt but never telling them the price per bag.
we’re not training clinicians. we’re training guessers with stethoscopes.
Richard Elias
November 30, 2025 AT 22:41of course doctors dont know prices. theyre too busy being heroes to check the damn bill. meanwhile patients are choosing between insulin and rent. this isnt a system failure - its a moral failure. fix the system or stop pretending you care.
Scott McKenzie
December 2, 2025 AT 08:00just saw this in my clinic yesterday - patient was prescribed a $300 med. turned out they could get the same thing at Walmart for $12. they had no idea.
we need real-time cost pop-ups. like a price checker for meds. 🛒💊
its not hard. its just not prioritized.
Jeremy Mattocks
December 2, 2025 AT 09:02listen, this isn’t just about prescriptions - it’s about how broken our entire healthcare model is. we treat medicine like a luxury product instead of a basic human right. doctors are stuck in the middle - they want to help, but they’re handed a system that’s designed to confuse, delay, and bankrupt people.
medical schools need mandatory courses on pharmaceutical economics, insurance tiers, copay assistance programs, and how PBMs screw patients over. it’s not optional anymore. people are dying because we pretend this isn’t part of clinical care.
and don’t even get me started on how pharmacies can charge $320 for the same pill that’s $15 down the street. that’s not capitalism - that’s corporate extortion.
we’ve got the tech. we’ve got the data. we’ve got the studies. what we don’t have is the will to fix it.
and until we stop treating cost as a "social issue" and start treating it as a clinical variable - this will keep happening. every single day. to someone’s mother. someone’s brother. someone’s kid.
Paul Baker
December 3, 2025 AT 08:18why is this even a thing 🤦♂️
we have apps that tell you the price of gas across 50 miles but cant tell you if your med costs 5 bucks or 500
its wild
Zack Harmon
December 4, 2025 AT 03:53THIS IS A MASSACRE. a MEDICAL MASSACRE.
doctors are playing Russian roulette with prescriptions and no one’s even noticed the gun is loaded.
patients are dying because someone thought a statin was $10 instead of $320 and now their heart’s done.
and the system? it shrugs. "oh well, we tried."
NO. YOU DIDN’T TRY. YOU JUST GAVE UP.
if your kid needed insulin and you couldn’t afford it - would you blame the doctor? then why do you let them keep guessing?
Jeremy S.
December 4, 2025 AT 22:56we need to stop acting like price is a separate issue. it’s part of the diagnosis. if the drug doesn’t fit the patient’s budget, it doesn’t fit the patient. period.
Jill Ann Hays
December 6, 2025 AT 18:20the fundamental epistemological flaw lies in the ontological separation of clinical efficacy from economic accessibility. the biomedical paradigm has been structurally insulated from market realities since the 1980s. until this Cartesian dualism is dismantled, pharmacological outcomes will remain contingent on socioeconomic privilege rather than therapeutic necessity
Mike Rothschild
December 7, 2025 AT 22:43my dad’s a retired cardiologist. he told me he used to write prescriptions without a second thought about cost. then his own wife had to choose between her meds and groceries. he cried for a week.
now he asks every patient: "can you afford this?"
simple. human. effective.
we just need to make it standard.
Tionne Myles-Smith
December 8, 2025 AT 02:13thank you for writing this. i’ve been screaming about this for years. my cousin took half her insulin because she couldn’t afford the other half. she ended up in the ER. again. again. again.
doctors need to be able to say: "here’s the $5 option that works just as well."
but they can’t. because they don’t know.
and that’s on all of us for letting it slide.
Leigh Guerra-Paz
December 8, 2025 AT 03:18oh my gosh, this is so important! I’ve seen this so many times in my work as a nurse - patients crying because they’re skipping doses, cutting pills, or just not filling the script because they’re scared of the bill.
and the doctors? they’re not being careless - they’re just not trained to think about it. it’s not their fault. it’s the system.
but we can fix it! We can push for real-time pricing in EHRs, we can demand that med schools teach this stuff, we can ask our reps to support transparency laws.
it’s not hopeless - it’s just been ignored for too long.
please, let’s not look away anymore. ❤️
Jordyn Holland
December 8, 2025 AT 20:01oh please. doctors are just lazy. if they cared, they’d look it up. this isn’t a system problem - it’s a character problem. they’re too busy being "heroes" to do the bare minimum of checking a price.
and don’t even get me started on how patients expect free medicine while complaining about taxes.
someone needs to tell them: life isn’t fair. take your $320 statin or don’t.
ABHISHEK NAHARIA
December 10, 2025 AT 10:56in india we dont have this problem because medicines are cheap. why do americans pay so much? because you have greedy pharma companies and lazy doctors who dont care about poor people. this is capitalist exploitation. you need to fix your system not blame doctors
Hardik Malhan
December 11, 2025 AT 03:23the lack of integration between payer-specific formularies and clinical decision support systems represents a critical interoperability gap in ambulatory care workflows. without standardized API-level access to real-time out-of-pocket cost data derived from patient-specific insurance parameters, cost-conscious prescribing remains a theoretical construct rather than an actionable clinical protocol