DRESS syndrome is one of the most dangerous drug reactions you’ve never heard of. It doesn’t show up right away. It doesn’t always look like a typical allergy. And if you miss it, it can shut down your liver, kidneys, or even kill you. Yet, it’s often mistaken for the flu, a viral rash, or a simple skin irritation. In Australia alone, an estimated 300 to 500 cases occur each year - and nearly half of them are misdiagnosed in the first week.
What DRESS Syndrome Actually Is
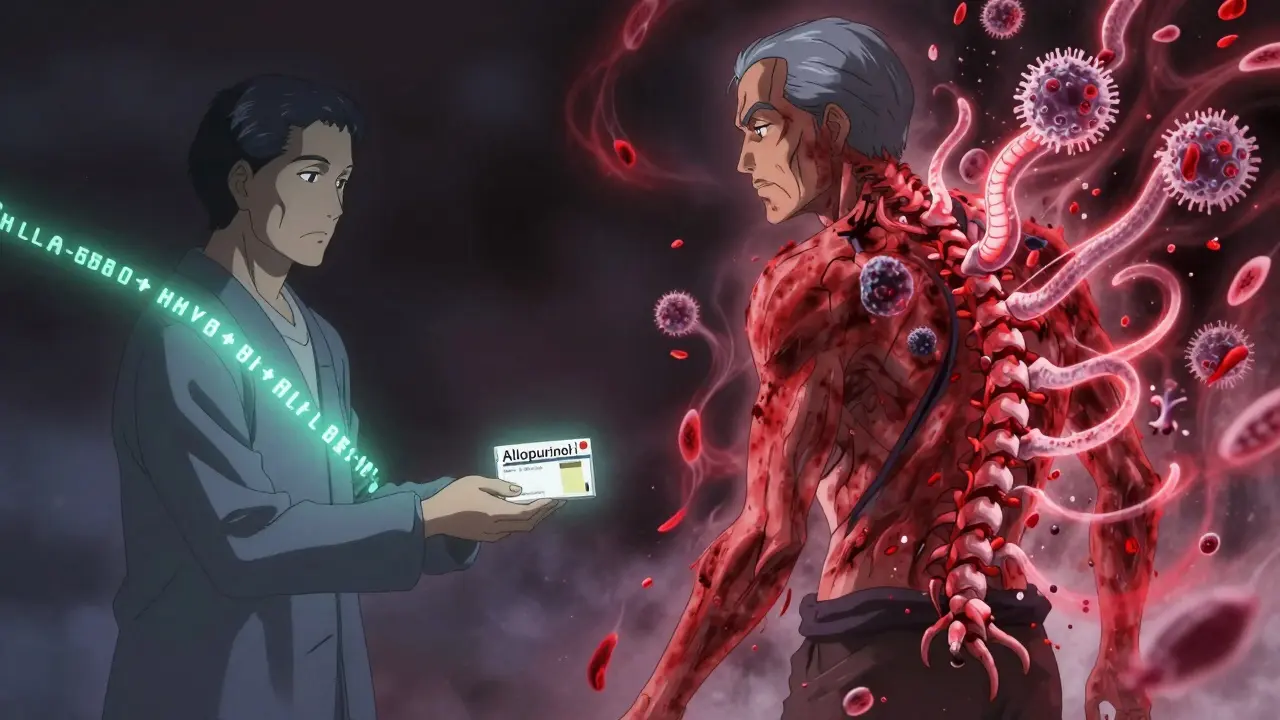
DRESS stands for Drug Reaction with Eosinophilia and Systemic Symptoms. It’s not just a rash. It’s a full-body immune meltdown triggered by certain medications. The body doesn’t just react - it overreacts. White blood cells called eosinophils, which normally fight parasites, go wild. They attack your organs. At the same time, your immune system turns on itself, sometimes triggering autoimmune diseases months after the rash is gone.
Unlike hives or mild rashes that fade in days, DRESS takes weeks to show up. Most people start feeling off 2 to 8 weeks after starting a new drug. That’s why doctors often don’t connect the dots. You’ve been on the medication for a month. You’re not thinking it’s the cause. But that delay is deadly.
How It Starts - The Early Warning Signs
It begins like a bad cold. Fever above 38°C. Sore throat. Swollen glands. You feel exhausted. You think you’ve caught the flu. Maybe you’ve been working too hard. Or maybe you’re just coming down with something.
Then, within a day or two, the rash appears. It’s not raised or itchy like an allergy. It’s flat, red, and spread out - like measles. About 80% of cases look like this. Some people get blisters. Others have purple spots. The rash covers large areas - chest, back, face, arms. It doesn’t go away with antihistamines. It gets worse.
At this point, most patients go to their GP. They get told it’s a virus. Or they’re given more antihistamines. Or worse - they’re told to keep taking the medication. That’s when things spiral.
The Organ Damage You Can’t See
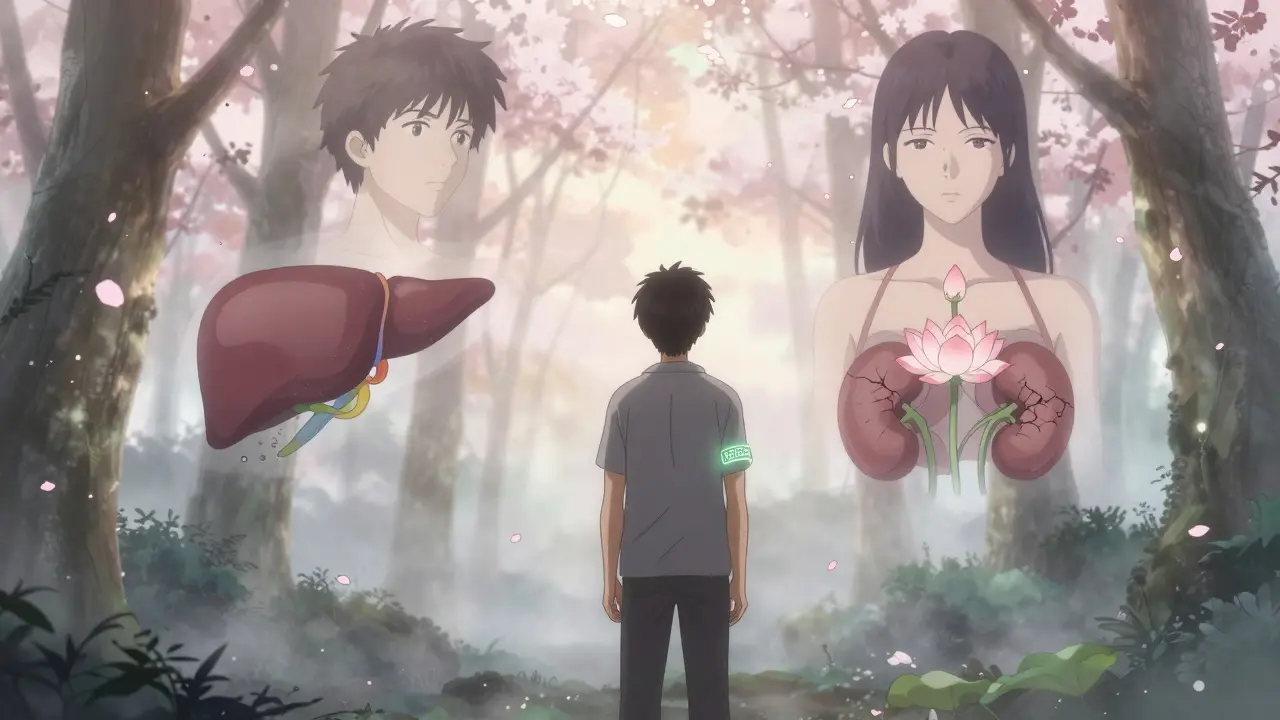
DRESS isn’t just skin deep. It’s a systemic disaster. In 70 to 90% of cases, the liver is damaged. ALT and AST levels - the markers of liver health - can spike to over 1,000 U/L. Normal is under 40. Some patients have liver enzymes higher than 3,000. That’s not inflammation. That’s necrosis. Liver failure.
Kidneys take a hit in 10 to 30% of cases. Creatinine rises. Urine output drops. Some need dialysis. Lungs get inflamed. Blood counts go haywire. Eosinophils climb above 1,500 per microliter. Normal is under 500. Atypical lymphocytes flood the bloodstream. You’re not just sick - your immune system is in chaos.
And here’s the twist: 60 to 70% of DRESS patients reactivate a hidden virus - HHV-6. It’s a herpes virus most people carry silently. But when your immune system is thrown off by a drug, it wakes up. And it makes the reaction worse. That’s why some patients get worse after they stop the drug. The virus is still there.
Which Drugs Cause DRESS?
Not every drug causes this. But some are notorious. The top three culprits are:
- Allopurinol - used for gout. Responsible for 40 to 50% of all DRESS cases. If you have kidney disease, your risk jumps 20-fold.
- Antiepileptics - carbamazepine, phenytoin, lamotrigine. These are common in older adults and people with nerve pain or epilepsy.
- Sulfonamides - antibiotics like sulfamethoxazole (Bactrim). Often prescribed for UTIs or sinus infections.
Other triggers include some antivirals, NSAIDs, and even a few psychiatric drugs. The key isn’t the drug class - it’s your genetics. If you’re of Asian descent, you carry the HLA-B*58:01 gene. That single gene increases your risk of allopurinol-induced DRESS by 55 times. That’s why Taiwan now requires a blood test before prescribing allopurinol. Australia doesn’t yet - but it should.
DRESS vs. SJS/TEN - Why the Difference Matters
Doctors often confuse DRESS with Stevens-Johnson Syndrome (SJS) or Toxic Epidermal Necrolysis (TEN). But they’re not the same.
SJS and TEN cause skin to peel off like a burn. They happen fast - within days. Mucous membranes (mouth, eyes, genitals) are destroyed. Mortality is high - up to 40% for TEN.
DRESS? The skin doesn’t peel. Mucous membranes are rarely involved. It’s slower. But it attacks your organs. And the death rate? Around 10%. Still deadly. But preventable.
The biggest difference? Eosinophils. SJS/TEN are driven by killer T-cells. DRESS is driven by eosinophils and CD4+ T-cells. That’s why steroids work for DRESS - they calm eosinophils. They don’t help SJS/TEN as much.
Diagnosis Is a Puzzle - Here’s How to Solve It
There’s no single blood test for DRESS. Diagnosis is based on a checklist - the RegiSCAR criteria. You need hospitalization plus at least three of these:
- Fever over 38°C
- Skin rash
- Swollen lymph nodes
- Eosinophils above 1,500/μL or over 10% of white blood cells
- Atypical lymphocytes in the blood
- Involvement of at least three internal organs (liver, kidneys, lungs, heart, pancreas)
Doctors also check for HHV-6 reactivation. A PCR test on blood can confirm it. It’s not required for diagnosis - but it helps. If HHV-6 is active, the illness is likely to be longer and more severe.
Here’s the problem: only 35% of internal medicine residents can correctly identify DRESS. That’s not a patient problem. That’s a system failure. If you’ve been on a high-risk drug for more than two weeks and suddenly develop fever and rash - demand a full blood count with differential. Ask: “Could this be DRESS?”
What Happens If You Don’t Act Fast
Delay kills. If you stop the drug within 24 hours of noticing symptoms, your chance of dying drops from 15% to 5%. That’s not a small difference. That’s life or death.
But stopping the drug is just step one. You need hospital care. Most patients stay 14 to 21 days. Why? Because organs keep failing even after the drug is gone. Liver enzymes can keep rising for days. Kidney function can crash. Infections set in - bacteria, fungi. One patient in a 2022 case report developed bloodstream infections from E. coli and Candida because their skin barrier was compromised.
Treatment? High-dose steroids. Prednisone at 0.5 to 1 mg per kg per day. That’s 50 to 100 mg daily for a 70kg person. It’s not gentle. But it saves lives. Tapering takes 4 to 8 weeks. Too fast? The rash and fever come back. Too slow? You get diabetes, bone loss, or infections from the steroids themselves.
New treatments are emerging. Anakinra, a drug used for rheumatoid arthritis, has cut hospital stays by over a week in trials. Tocilizumab, used for severe arthritis, is being tested for steroid-resistant cases. These aren’t cures - but they’re hope.
Long-Term Damage - The Hidden Cost
Even if you survive, DRESS leaves scars. Not on your skin - inside your body.
One in five patients develops an autoimmune disease after DRESS. Graves’ disease. Lupus. Type 1 diabetes. In one Reddit case, a man developed thyroid cancer five years after carbamazepine-induced DRESS. It’s rare - but it happens.
A survey of 150 DRESS survivors found 27% needed ongoing kidney care. One in three had abnormal liver tests six months later. Some never fully recover.
And the emotional toll? Massive. Patients report anxiety, PTSD, and fear of all medications. One woman told her story on the NORD forum: “I won’t take any new pill unless I’m in the hospital. Even aspirin scares me.”
How to Protect Yourself
If you’re on allopurinol and have kidney disease - talk to your doctor. Ask if you’ve been tested for HLA-B*58:01. If you’re Asian and on carbamazepine - ask the same. These tests are cheap. They’re fast. And they prevent death.
If you’re prescribed a new drug - especially one of the big three - know the signs. Fever + rash after two weeks? Don’t wait. Go to the ER. Say: “I think this might be DRESS.”
Keep a list of every medication you’ve taken in the last three months. Bring it with you. Show it to every doctor. Most patients see three or more doctors before getting the right diagnosis. Don’t be one of them.
And if you’ve had DRESS - never take the drug again. Not even once. Cross it off your list. Tell every future doctor. Write it on your medical alert bracelet. This reaction doesn’t get milder. It gets worse.
What’s Changing - And What You Should Watch For
More doctors are learning. In 2023, the American College of Rheumatology recommended febuxostat over allopurinol for patients with kidney disease. That’s a game-changer. It could prevent 1,200 DRESS cases a year in the U.S. alone.
Europe is rolling out a new diagnostic tool - a point-of-care test that checks for eosinophil proteins and HHV-6 in under an hour. It’s not in Australia yet. But it’s coming.
The number of DRESS cases is rising. Why? Because we’re giving more of these drugs to older people. More gout. More seizures. More chronic pain. More prescriptions. And we’re not screening.
By 2030, DRESS cases could rise 25%. That’s not speculation. It’s a projection from global rheumatology data. We’re not ready.
But you can be. Know the signs. Ask the questions. Speak up. DRESS doesn’t care how smart you are. It only cares if you’re awake.


