Lupus Pulmonary Embolism Risk Calculator
Lupus Pulmonary Embolism Risk Assessment
This tool helps you understand your risk of developing a pulmonary embolism based on lupus-specific factors. Your results will help you discuss risk management with your healthcare provider.
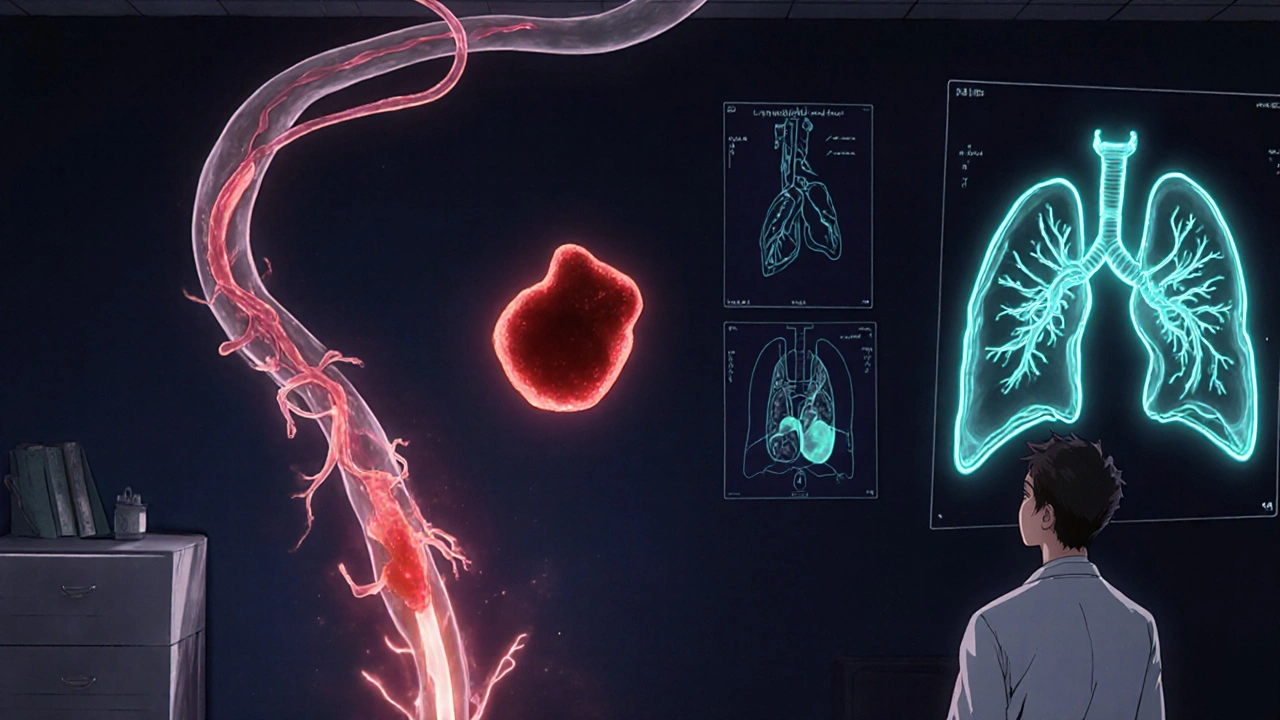
When an autoimmune disease like Systemic Lupus Erythematosus is a chronic condition where the immune system attacks healthy tissue collides with a life‑threatening clot in the lungs, the outcome can be frightening. This article unpacks why people with lupus face a higher chance of developing a Pulmonary Embolism, what symptoms to watch for, and how doctors and patients can lower the danger.
What Is Systemic Lupus Erythematosus?
Lupus is an Autoimmune Disease that affects roughly 5 million people worldwide. The immune system creates auto‑antibodies that damage skin, joints, kidneys, the brain, and, crucially for this discussion, the blood vessels. Flares can swing from mild skin rashes to severe organ failure.
Understanding Pulmonary Embolism
A pulmonary embolism (PE) occurs when a blood clot travels to the lungs and blocks a pulmonary artery, cutting off oxygen to lung tissue. Commonly the clot originates as a deep‑vein thrombosis (DVT) in the legs, then migrates upward. Symptoms range from sudden shortness of breath to chest pain, rapid heartbeat, or even collapse.
Why Lupus Increases PE Risk
Several mechanisms link lupus to clot formation:
- Antiphospholipid Antibody Syndrome (APS): Up to 40 % of lupus patients develop antiphospholipid antibodies that make blood more “sticky.”
- Inflammation: Chronic inflammation damages the lining of blood vessels, encouraging clotting.
- Medication side effects: High‑dose steroids raise cholesterol and triglyceride levels, both clot promoters.
- Immobility: Joint pain can limit activity, a classic DVT trigger.
These factors combine to make the lupus pulmonary embolism risk substantially higher than in the general population.
Key Risk Factors - Lupus vs. General Population
| Risk Factor | General Population | Lupus Patients |
|---|---|---|
| Age > 60 | High | Moderate - younger patients still at risk due to disease |
| Obesity | High | High - steroids often increase weight |
| Smoking | High | High - additive with inflammation |
| Recent surgery or trauma | High | High - plus disease‑related immobility |
| Antiphospholipid antibodies | Low | High - present in 30‑40 % of lupus cases |
| Active disease flare | Low | High - inflammation spikes clotting risk |
Typical Signs & Symptoms to Spot Early
Because lupus can mask or mimic many ailments, PE symptoms may be dismissed. Keep an eye out for:
- Sudden shortness of breath that doesn’t improve with rest
- Sharp chest pain that worsens when breathing in
- Rapid heart rate (over 100 bpm)
- Light‑headedness, fainting, or sudden weakness
- Unexplained cough, sometimes with blood‑streaked sputum
If any of these appear during a lupus flare, seek medical care immediately.
How Doctors Diagnose a PE in Lupus Patients
- Clinical assessment - review symptoms, recent flares, medication history.
- Blood tests - D‑dimer levels are often elevated but can be falsely high in lupus; a markedly high result still pushes the work‑up forward.
- Imaging - a CT pulmonary angiography (CTPA) is the gold standard. For patients with kidney involvement, a ventilation‑perfusion (V/Q) scan may be preferred.
- Ultrasound of the legs - to find an underlying DVT.
- Antiphospholipid testing - lupus anticoagulant, anticardiolipin, and anti‑β2‑glycoprotein I antibodies guide long‑term therapy.
These steps ensure that clinicians differentiate a clot from lupus‑related lung inflammation.
Treatment Options - From Acute Care to Long‑Term Management
Once a PE is confirmed, treatment follows two tracks:
- Acute phase: Anticoagulant Therapy with low‑molecular‑weight heparin (LMWH) or unfractionated heparin is started immediately. In severe cases, thrombolytic drugs may be used.
- Maintenance phase: Transition to oral anticoagulants such as warfarin (target INR 2.0‑3.0) or direct oral anticoagulants (DOACs) if no contraindications exist. For patients with confirmed APS, lifelong anticoagulation is often recommended.
Physicians also adjust lupus‑specific meds - tapering high‑dose steroids, adding hydroxychloroquine (which may reduce clot risk), or switching to steroid‑sparing agents like mycophenolate.

Preventive Strategies You Can Adopt
Prevention is a partnership between you and your care team. Practical steps include:
- Regular screening: Annual antiphospholipid antibody panels for anyone with active lupus.
- Stay active: Gentle low‑impact exercise (walking, swimming) combats immobility without stressing joints.
- Maintain a healthy weight: Work with a dietitian to manage steroid‑induced weight gain.
- Quit smoking: Even occasional tobacco magnifies clot risk.
- Hydration: Dehydration thickens blood, especially during flares.
- Medication adherence: Never skip anticoagulants; set alarms or use pill organizers.
During hospital stays or after surgery, ask your doctor about prophylactic compression stockings or short‑term heparin shots.
When to Call Emergency Services
Time is vital. Dial 911 if you experience:
- Sudden, severe shortness of breath
- Chest pain that worsens with deep breaths
- Rapid, irregular heartbeat
- Fainting or extreme dizziness
Even if you’re already on anticoagulants, a new clot can develop.
Future Directions - Research and Hope
Scientists are exploring targeted therapies that block specific inflammatory pathways without broad immunosuppression. Early trials of complement inhibitors show promise in reducing both lupus activity and clot formation. Meanwhile, improved DOAC formulations aim to simplify lifelong anticoagulation for APS patients.
Staying informed about clinical trials and discussing them with your rheumatologist can give you access to cutting‑edge care.
Quick Recap
- Lupus creates a pro‑clot environment via antiphospholipid antibodies and chronic inflammation.
- Symptoms of PE can overlap with lupus flares, so vigilance is key.
- Diagnosis blends blood tests, imaging, and antibody screening.
- Treatment starts with heparin, moves to long‑term anticoagulation, and includes lupus‑specific medication adjustments.
- Prevention hinges on lifestyle, regular screening, and strict medication adherence.
Can lupus cause a blood clot in the lungs?
Yes. Lupus‑related antibodies and inflammation increase the odds of deep‑vein thrombosis, which can travel to the lungs as a pulmonary embolism.
What is the most reliable test for detecting a PE?
A CT pulmonary angiography (CTPA) is considered the gold standard because it directly visualizes clots in the pulmonary arteries.
Should every lupus patient be on blood thinners?
Not automatically. Only those with a history of clotting, confirmed antiphospholipid syndrome, or a recent PE are typically prescribed long‑term anticoagulants.
How can I tell if my shortness of breath is from lupus or a PE?
Lupus‑related lung issues usually develop gradually, while PE causes sudden, sharp breathlessness that worsens quickly. If it appears abruptly, seek emergency care.
Are DOACs safe for lupus patients with antiphospholipid syndrome?
Current guidelines suggest warfarin remains the preferred option for high‑risk APS, but ongoing studies are evaluating specific DOACs for safety.



Selina M
October 23, 2025 AT 21:45Hey there! If you’re looking to stay active even on a bad lupus day, just 10‑minute walks can keep the blood flow moving.
tatiana anadrade paguay
October 24, 2025 AT 19:46That’s a great start-pair those short walks with gentle stretching, and make sure you hydrate before and after; consistency really helps reduce clot risk over time.
Kristin Violette
October 25, 2025 AT 17:48The pathophysiological interplay between systemic lupus erythematosus (SLE) and thromboembolic phenomena is mediated principally by antiphospholipid antibodies (aPL), which precipitate a hypercoagulable milieu via endothelial activation and upregulation of tissue factor expression.
Subsequent platelet aggregation is amplified by complement cascade dysregulation, a hallmark of lupus flares, further augmenting the risk of deep‑vein thrombosis.
Epidemiological data indicate that approximately one‑third of SLE cohorts harbor clinically significant aPL, translating into a relative risk increase for pulmonary embolism that exceeds fourfold compared with age‑matched controls.
Moreover, chronic glucocorticoid exposure contributes to dyslipidemia and endothelial dysfunction, synergistically interacting with inflammatory cytokines such as IL‑6 and TNF‑α to potentiate clot formation.
In the acute diagnostic workup, D‑dimer assays lack specificity in lupus owing to baseline elevations; therefore, clinicians must interpret values in conjunction with imaging modalities.
Computed tomography pulmonary angiography (CTPA) remains the gold standard, offering high‑resolution visualization of segmental perfusion defects, whereas ventilation‑perfusion (V/Q) scanning is preferable in patients with compromised renal function due to contrast nephropathy concerns.
From a therapeutic standpoint, low‑molecular‑weight heparin (LMWH) is favored for immediate anticoagulation, given its predictable pharmacokinetics and reduced monitoring burden relative to unfractionated heparin.
Transition to long‑term oral anticoagulants necessitates individualized target INR ranges, especially in the presence of confirmed APS where a target of 2.5–3.5 may be endorsed.
Recent trials have explored direct oral anticoagulants (DOACs) in APS, yet data remain inconclusive, prompting many guidelines to retain warfarin as the preferred agent for high‑risk phenotypes.
Adjunctive rheumatologic management-optimizing hydroxychloroquine dosing and employing steroid‑sparing agents such as mycophenolate mofetil-can attenuate systemic inflammation and indirectly mitigate thrombotic propensity.
Lifestyle modifications, including consistent low‑impact aerobic exercise, smoking cessation, and vigilant hydration, serve as non‑pharmacologic pillars in embolism prophylaxis.
Patient education on early symptom recognition-sudden dyspnea, pleuritic chest pain, tachycardia-cannot be overstated, as time‑sensitive interventions dramatically improve outcomes.
Interdisciplinary coordination between rheumatology, hematology, and pulmonology ensures comprehensive risk stratification, particularly when considering prophylactic compression devices during periods of immobility.
Future research avenues involve complement inhibition (e.g., C5a receptor antagonists) which may concurrently dampen lupus activity and coagulopathy, representing a promising therapeutic nexus.
In summary, the confluence of immunologic, pharmacologic, and behavioral factors renders SLE patients uniquely susceptible to pulmonary embolism, mandating a multifaceted, proactive management paradigm.
Theo Asase
October 26, 2025 AT 14:50All this “guidelines” are just a smokescreen; the pharma‑big‑three push anticoagulants to lock patients into lifelong medication cycles while they skim the profit margins, and the real cure is being buried under layers of bureaucracy.
Joey Yap
October 27, 2025 AT 12:51When you step back and contemplate the fragile balance between our immune defenses and the coagulation cascade, you realize that lupus is less a disease and more a reminder of how interconnected our bodily systems truly are.
Lisa Franceschi
October 28, 2025 AT 10:53Indeed, a measured approach that respects patient autonomy while adhering to evidence‑based protocols is essential for optimal outcomes.
Diane Larson
October 29, 2025 AT 08:55For anyone on hydroxychloroquine, keep your quarterly eye exams up to date; retinal toxicity can sneak up, and preserving vision is just as important as preventing clots.
Michael Kusold
October 30, 2025 AT 06:56yeah, stay hydrated.
Jeremy Lysinger
October 31, 2025 AT 04:58Short walks + water = big win against clot risk.
Nelson De Pena
November 1, 2025 AT 03:00Maintaining a target INR of 2.5‑3.0 when on warfarin significantly lowers recurrent embolism rates.
Wilson Roberto
November 2, 2025 AT 01:01Understanding the cultural context of lupus care can improve adherence; patients from diverse backgrounds may have differing beliefs about medication, so culturally sensitive communication is key.
Taylor Nation
November 2, 2025 AT 23:03Let’s all share our personal coping strategies-whether it’s yoga, meditation, or a favorite playlist-to build a supportive community that tackles both flare-ups and clot prevention together.
Brian Klepacki
November 3, 2025 AT 21:05The medical literature is saturated with buzzwords and hollow recommendations, masking the harsh reality that many clinicians still overlook the silent threat of pulmonary embolism until it becomes a catastrophic event.
Katherine Collins
November 4, 2025 AT 19:06meh, read the article… not that exciting :)