For millions of Medicare beneficiaries, the cost of daily medications used to be a hidden tax on aging. Before 2025, someone taking a few generic pills every day could easily spend thousands out of pocket before their drug coverage kicked in fully. Now, thanks to major changes under the Inflation Reduction Act, Medicare Part D is delivering real savings - especially for people relying on generic drugs.
What Changed in Medicare Part D in 2025?
The biggest shift? The out-of-pocket cap for prescription drugs dropped from nearly $8,000 to just $2,000. That means once you’ve paid $2,000 in eligible costs for your meds in a year, you pay nothing for the rest of the year - no matter how many prescriptions you fill. This change alone saved Part D enrollees an estimated $7.4 billion in 2025, according to the Centers for Medicare & Medicaid Services (CMS).
Generics make up 84% of all prescriptions filled under Part D, but they used to account for only 27% of total spending. Why? Because even cheap drugs added up when patients paid full price before hitting the old, high cap. Now, with the $2,000 limit, those small daily costs stop adding up after a point. If you take a $10 generic blood pressure pill every day, you’ll hit the cap in about 200 days - and after that, your next 150 prescriptions cost $0.
How Copays Work for Generics in 2025
Medicare Part D plans still have a structure: deductible, initial coverage, coverage gap (donut hole), and catastrophic coverage. But the rules changed.
- Deductible: Up to $590 in 2025 - but many plans, especially Medicare Advantage plans, have $0 deductibles.
- Initial Coverage: After the deductible, you pay 25% coinsurance for generics. Most preferred generics have a flat copay of $10 for a 30-day supply. That’s the same whether you’re in a stand-alone drug plan (PDP) or a Medicare Advantage plan (MA-PD).
- Catastrophic Coverage: Once you hit $2,000 in out-of-pocket spending, you pay $0 for all covered drugs for the rest of the year. This includes generics and brand-name drugs alike.
Here’s the catch: only certain payments count toward that $2,000 cap. Your monthly premium doesn’t count. But your deductible, copays, coinsurance, and even manufacturer discounts do. Many people don’t realize that the $5 discount a drugmaker gives on a $40 generic still counts as $5 toward their cap. That’s why someone might hit the cap faster than they expect.
PDPs vs. MA-PDs: Which Saves More on Generics?
There are two main ways to get Part D coverage: Stand-alone Prescription Drug Plans (PDPs) and Medicare Advantage Prescription Drug plans (MA-PDs). They cover the same drugs, but their costs look very different.
| Feature | Stand-Alone PDP | Medicare Advantage (MA-PD) |
|---|---|---|
| Average Monthly Premium | $39 | $7 |
| Median Generic Copay (30-day) | $10 | $10 |
| Annual Deductible (Common) | 85% have one | 60% have one |
| Total Annual Out-of-Pocket Cap | $2,000 | $2,000 |
| Extra Benefits (e.g., dental, vision) | No | Often included |
On the surface, copays are the same. But if you’re paying $39 a month for a PDP, that’s $468 a year - and none of it counts toward your $2,000 cap. Meanwhile, an MA-PD might charge $7 a month for drug coverage, meaning you’re paying $84 a year - and you’re probably getting vision, dental, or fitness benefits too. For someone on fixed income, that difference matters.

Who Saves the Most?
People taking multiple generics save the most. If you’re on three or four daily medications - say, for blood pressure, cholesterol, and diabetes - you’re likely to hit the $2,000 cap by mid-year. After that, your meds are free. One Reddit user, a retired pharmacist, shared: “My generic blood pressure meds now cost me $0 after hitting the $2,000 cap. Last year, I paid $1,200 more for the same drugs.”
Low-income beneficiaries get even more help. If you qualify for Extra Help (Low-Income Subsidy), you pay $0 deductible and $0-$4.50 copays for generics. No cap to hit - you’re protected year-round.
But not everyone benefits equally. People on brand-name drugs with high list prices still face higher costs in the initial phase, and some plans restrict access to certain generics through prior authorization or step therapy. The Accessible Medicines Foundation found Part D plans use more restrictions on generics than commercial insurers. That means even if a drug is generic, your plan might make you try another one first - and that can delay care.
Why Some People Are Still Confused
The system is simpler now, but it’s still complex. A KFF study found 41% of beneficiaries didn’t understand how manufacturer discounts counted toward the $2,000 cap. Others didn’t know that their copays on a $5 generic still counted - even if they didn’t pay it out of pocket because their plan negotiated it down.
Medicare’s Plan Finder tool helps you compare plans, but a 2024 GAO report showed 32% of users needed help navigating it. If you’re on multiple generics, plug them into the tool. Look for plans with low copays, no deductible, and high formulary coverage. Don’t just pick the cheapest premium - check the total cost of your meds.
What’s Next? The Future of Generics in Part D
The 2025 reforms are just the start. In 2026, a new program will give PDPs a 10% subsidy for high-cost generics, which could lower copays even more. Biosimilars - generic versions of complex biologic drugs - are also starting to appear. By 2028, they could cover 35% of the biologic market, bringing more savings.
But there’s a risk. Because Medicare now pays less reinsurance for generics after the $2,000 cap, some plans might push back by limiting which generics they cover or requiring more steps before approving them. Experts like Dr. Stacie Dusetzina warn that “the shift in reinsurance responsibility may lead some plans to increase formulary restrictions on high-cost generics.”
Still, the overall trend is clear: generics are now the most powerful tool for cutting drug costs under Medicare. With 87% of Part D prescriptions expected to be generics by 2028, and the $2,000 cap protecting everyone, the system is finally aligned with what patients need - affordable, predictable costs.
What You Should Do Now
- Log into Medicare.gov and use the Plan Finder tool. Enter your exact medications - including generics - and compare plans side by side.
- Check if you qualify for Extra Help. Even if you think your income is too high, the limits are higher than most people realize. Apply at SSA.gov.
- Don’t assume your current plan is still the best. Premiums and formularies change every year. Open enrollment ends December 7, 2025 - so act fast if you’re thinking of switching.
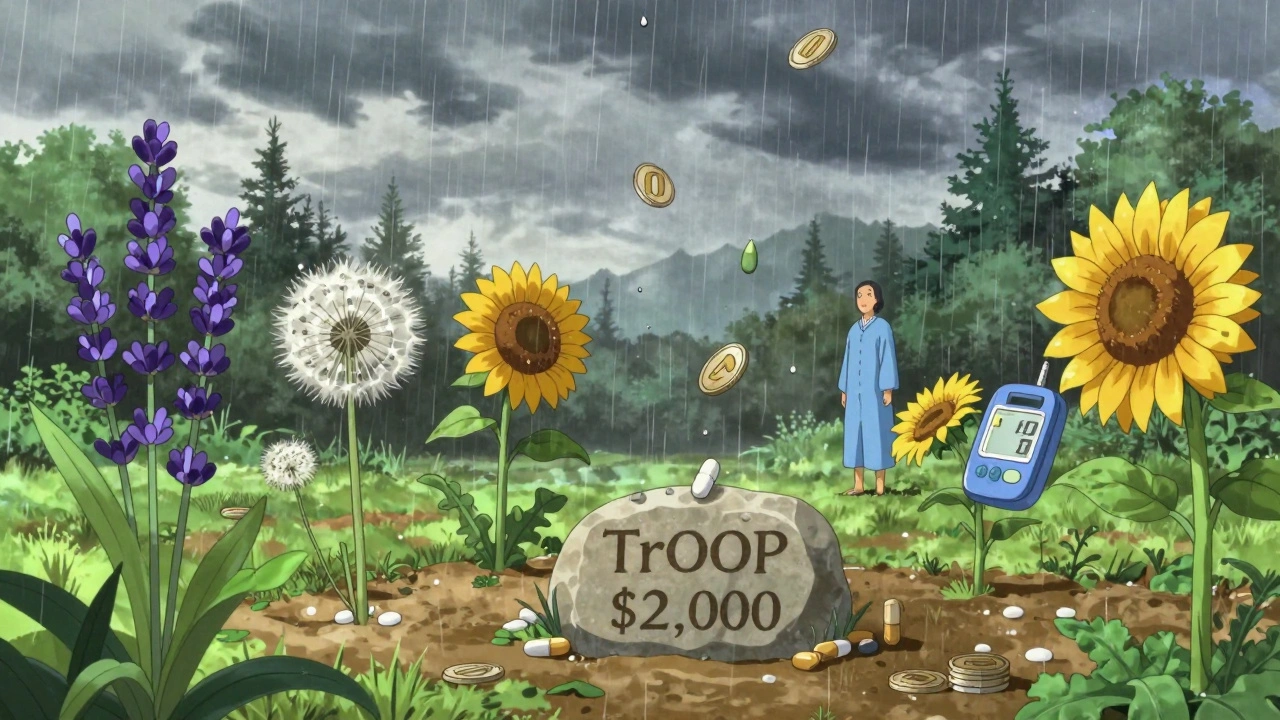
- Keep all your receipts. Even small copays count toward your $2,000 cap. If you think you’ve hit it, call your plan and ask for a TrOOP (True Out-of-Pocket) statement.
The goal isn’t just to pay less. It’s to stop worrying about whether you can afford your next pill. For millions, that’s finally becoming real.
Do generic drugs cost less in Medicare Part D in 2025?
Yes. In 2025, the median copay for a 30-day supply of a preferred generic drug is $10 across most Part D plans. After you spend $2,000 out of pocket in a year, your generic drugs cost $0 for the rest of the year. This is a major change from pre-2025 rules, where people often paid thousands before reaching full coverage.
Does my monthly premium count toward the $2,000 out-of-pocket cap?
No. Only what you pay for your drugs - including deductibles, copays, and coinsurance - counts toward the $2,000 cap. Monthly premiums don’t count, even if you’re paying $30 or $40 a month for your Part D plan. That’s why it’s important to look at total drug costs, not just premiums, when choosing a plan.
Can my Part D plan switch my generic drug without telling me?
Yes, but only under certain conditions. Many plans use step therapy or therapeutic substitution, meaning they may require you to try a different generic version first. If they change your medication, they must notify you in advance. You can appeal the change or request an exception if the new drug doesn’t work for you. Check your plan’s formulary each year - it changes frequently.
How do I know if I’ve hit the $2,000 out-of-pocket cap?
Your Part D plan sends you a statement called a TrOOP (True Out-of-Pocket) report, usually monthly or quarterly. It shows how much you’ve spent on covered drugs so far. You can also call your plan or log into your account on Medicare.gov to check your progress. Once you hit $2,000, your copays drop to $0 for the rest of the year - and you don’t need to do anything to activate it.
Do I qualify for Extra Help with my drug costs?
You may qualify if your income is below $21,870 for an individual or $29,580 for a couple in 2025, and your assets are under $17,220 (or $34,360 for a couple). Extra Help covers your deductible, lowers your copays to $0-$4.50 for generics, and eliminates the coverage gap. Apply at SSA.gov or call 1-800-772-1213. Many people who qualify don’t apply - so it’s worth checking.
Why are some generic drugs still expensive under Part D?
Some generics are priced higher because they’re complex to manufacture or have limited competition. Others are “non-preferred” on your plan’s formulary, meaning your plan puts them in a higher cost tier. Always check if there’s a preferred generic alternative - often, two generics for the same drug exist, and one costs much less. Your pharmacist can help you find it.
Should I switch from a PDP to an MA-PD to save on generics?
It depends. If you’re only taking generics and don’t need extra benefits, a PDP might be fine. But if you’re paying $39/month for a PDP and $7/month for an MA-PD, the savings add up fast - and MA-PDs often include dental, vision, or fitness perks. Compare total annual costs: premiums + copays. Many people save $1,000+ per year by switching. Use Medicare’s Plan Finder to compare.
Next Steps: Don’t Wait Until It’s Too Late
If you’re on Medicare and take any generic drugs, your best move right now is to review your plan. Open enrollment ends December 7, 2025. After that, you’re locked in until next year. Use the Plan Finder tool. Call your pharmacist. Ask your doctor if there’s a cheaper generic alternative. And if you’re struggling to pay, apply for Extra Help - it’s easier than you think.
Medicare Part D was designed to help people afford prescriptions. In 2025, it finally started working the way it should - especially for generics. Don’t let confusion or inertia cost you money you’ve already earned through decades of work. The savings are real. You just need to take one step to claim them.



Michael Robinson
December 10, 2025 AT 06:33It's wild how a simple cap can change everything. I used to skip doses just to make my pills last. Now? I take them like I'm supposed to. No guilt, no math, no stress. That's not policy - that's dignity.
They talk about savings like it's a number on a spreadsheet. But for folks like me? It's sleep at night.
Generics aren't cheap because they're weak. They're cheap because they work. And now, finally, the system gets it.
Andrea Petrov
December 11, 2025 AT 00:43Wait - you really believe the government didn’t engineer this? The cap drops right after Big Pharma’s lobbying peaked? Coincidence? The same people who pushed for 30-day supply limits now say ‘trust the system’?
Manufacturers get subsidies for discounts? That’s not saving money - that’s moving the goalposts. They’re still charging $100 for a $5 pill. They just let you think you’re winning.
Check your TrOOP statement next month. I bet your ‘$0’ copay comes with a formulary change next quarter. They always do.
Suzanne Johnston
December 12, 2025 AT 09:24I’ve spent years helping older patients navigate Part D, and this is the first time I’ve seen real relief. The $2,000 cap doesn’t just lower bills - it lowers anxiety. People stop choosing between insulin and groceries.
Yes, premiums don’t count. Yes, some plans restrict generics. But the core shift? It’s real. We’ve moved from ‘hope you make it to catastrophic’ to ‘you’re protected.’ That’s a moral win.
Don’t let the cynics drown out the human impact. I had a woman cry in my office last week because her metformin was free for the first time in 12 years. That’s not a statistic. That’s a life.
And yes, use Plan Finder. Even if you think you’re fine, you might be leaving $800 on the table. It takes 15 minutes. Do it.
Graham Abbas
December 14, 2025 AT 03:24OH MY GOD I JUST REALIZED I’M PAYING $0 FOR MY BLOOD PRESSURE MEDS NOW
I’VE BEEN TAKING LISINOPRIL FOR 7 YEARS AND LAST YEAR I SPENT $1,400 ON IT
THIS YEAR? I HIT THE CAP IN JULY AND NOW I’M GETTING IT FOR FREE
I WENT TO THE PHARMACY TO PICK IT UP AND THE PHARMACIST SAID ‘OH YOU’RE IN CATASTROPHIC’ AND I JUST STARTED LAUGHING AND CRYING AT THE SAME TIME
THIS IS WHAT POLITICS SHOULD LOOK LIKE. NOT TWEETS. NOT DEBATES. JUST PEOPLE GETTING THEIR MEDS.
PLEASE SHARE THIS WITH SOMEONE WHO STILL THINKS GOVERNMENT CAN’T HELP.
Haley P Law
December 15, 2025 AT 18:13OMG I JUST FIGURED OUT I’M SAVING OVER $1K THIS YEAR 😭😭😭
MY DIABETES MEDS USED TO COST ME $90 A MONTH 😭
NOW I PAY $10 UNTIL JULY AND THEN IT’S FREE 😍
MY GRANDMA SAID ‘YOU’RE LUCKY’ BUT I’M NOT LUCKY - I’M JUST NOT BROKE ANYMORE 😤
GO MEDI-CARE 😎💊
Andrea DeWinter
December 16, 2025 AT 18:25For anyone confused about the cap - here’s the quick version
Only what you pay out of pocket for meds counts - not your premium
Manufacturer discounts count too - so if your $40 pill has a $5 discount, that’s $5 toward your cap
Call your plan for your TrOOP statement - they send it monthly
Extra Help? Apply even if you think you don’t qualify - the limits are higher than you think
And always check your formulary - your ‘preferred’ generic might’ve changed
One phone call can save you hundreds
You got this
ian septian
December 17, 2025 AT 16:26Switched from PDP to MA-PD. Saved $400 on premiums alone. Copays same. Got free vision exam. Worth it.
Arun Kumar Raut
December 18, 2025 AT 03:16Back home in India, generics cost $1 a month. Here, $10 feels high - until you realize most Americans pay $50+ before this change.
The system isn’t perfect. But $2,000 cap? That’s a start.
Use Plan Finder. Talk to your pharmacist. Don’t wait. You’ve earned this.