Minimally Invasive Surgery Candidate Calculator
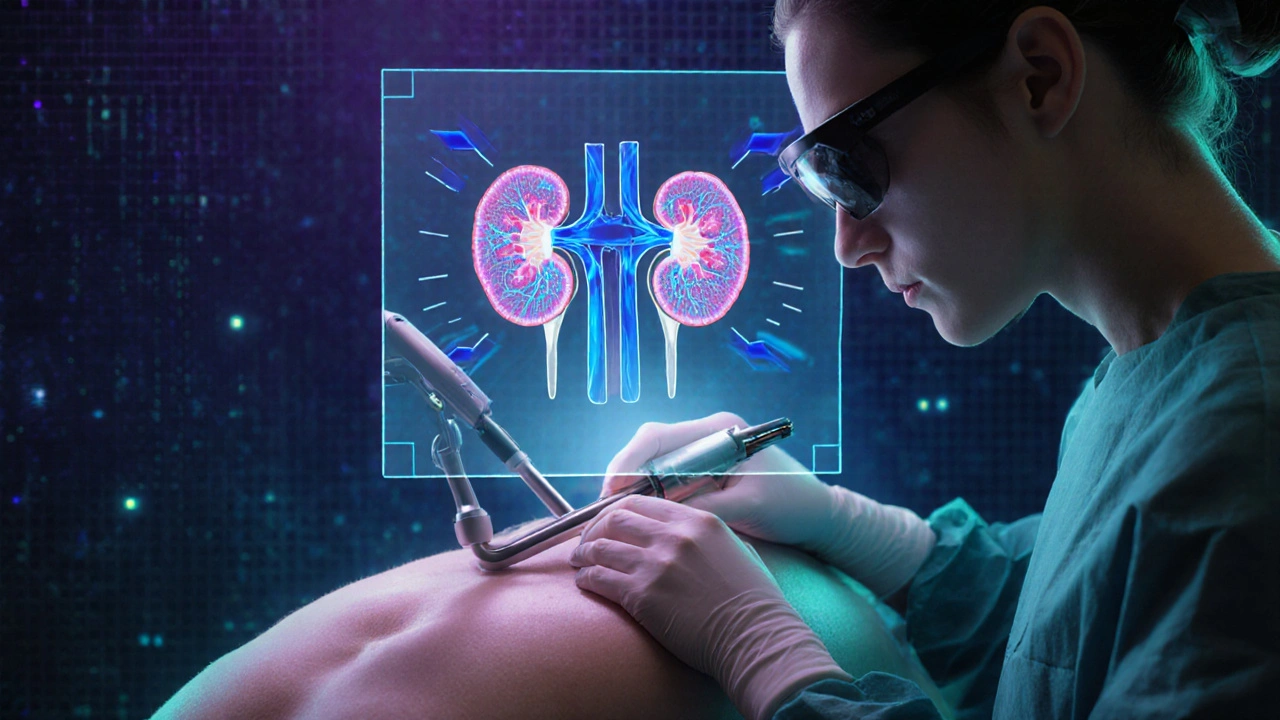
This calculator helps determine if minimally invasive surgery (MIS) is appropriate for advanced renal cell carcinoma based on key clinical factors. It uses criteria from recent studies and guidelines to estimate candidacy for laparoscopic or robotic approaches.
Patient Assessment
Enter the patient's key clinical characteristics to evaluate suitability for minimally invasive surgery.
Surgery Recommendation
Suggested modality:
When kidney cancer runs beyond the organ, many patients wonder if a small incision can still do the job. Minimally invasive surgery is a set of techniques that use tiny ports, cameras, and robotic arms to reach the tumor without opening the entire abdomen. For advanced renal cell carcinoma (RCC), the approach promises less pain, faster recovery, and, surprisingly, comparable cancer control when the right patients are chosen.
Key Takeaways
- Minimally invasive options-laparoscopic and robot‑assisted-are now standard for many stage III-IV RCC cases when the tumor is resectable.
- Patient selection hinges on tumor size, location, vascular involvement, and overall health.
- Evidence from 2023‑2025 trials shows similar overall survival to open surgery, with lower blood loss and shorter hospital stays.
- Enhanced Recovery After Surgery (ERAS) protocols amplify the benefits of MIS.
- Multidisciplinary planning remains essential; surgery is often combined with targeted therapy or immunotherapy.
Understanding Advanced Renal Cell Carcinoma
Renal cell carcinoma is the most common type of kidney cancer, representing about 85% of cases. When the disease spreads beyond the kidney (stage III or IV), it is labeled “advanced.” The TNM staging system grades the tumor (T), nodal involvement (N), and distant metastasis (M). Most advanced cases present with a T3/T4 tumor, regional lymph nodes, or limited lung and bone metastases.
Traditional management combined radical nephrectomy with systemic therapy. However, the rise of immune checkpoint inhibitors (e.g., nivolumab) and VEGF‑targeted agents (e.g., sunitinib) has shifted the treatment paradigm. Surgery now serves both as a cytoreductive tool (removing bulk disease) and as a bridge to systemic therapy.
Why Consider Minimally Invasive Surgery?
Open nephrectomy has been the gold standard for decades, but it carries a sizeable incision, higher postoperative pain, and longer convalescence. MIS techniques aim to reduce these drawbacks while preserving oncologic efficacy.
- Smaller incisions: Laparoscopic ports are typically 5-12mm; robotic arms require slightly larger (8-12mm) trocar sites.
- Reduced blood loss: Studies report a 30‑40% decrease compared with open surgery.
- Shorter hospital stay: Median LOS drops from 5‑7days (open) to 2‑3days (MIS).
- Faster return to systemic therapy: Patients can resume targeted or immunotherapy within 10‑14days, crucial for disease control.
These peri‑operative gains translate into better quality of life, especially for older adults or those with comorbidities.
Choosing the Right MIS Modality
Two main platforms dominate the field:
| Attribute | Laparoscopic | Robot‑Assisted | Open |
|---|---|---|---|
| Incision size | 5‑12mm ports | 8‑12mm ports + 2‑3cm assistant incision | 15‑30cm flank incision |
| Operative time | 150‑210min | 180‑240min (learning curve) | 120‑180min |
| Estimated blood loss | 150‑300mL | 100‑250mL | 400‑800mL |
| Complication rate (Clavien‑Dindo ≥III) | 5‑8% | 4‑7% | 12‑15% |
| Length of stay | 2‑3days | 2‑3days | 5‑7days |
| Oncologic equivalence (5‑yr OS) | ~55% (stage III) | ~57% (stage III) | ~54% (stage III) |
| Best suited for | Peripheral tumors ≤7cm, limited vascular involvement | Complex hilar lesions, partial nephrectomy in advanced disease | Masses requiring extensive vascular control or en‑bloc resection |
In practice, surgeons often start with laparoscopic techniques for straightforward cases and switch to robotic assistance when the tumor is deep‑seated or when a partial nephrectomy is desired despite advanced stage.
Patient Selection: Who Benefits Most?
A successful MIS case hinges on a careful pre‑operative work‑up:
- Imaging review: Multiphasic CT or MRI assesses tumor size, reniform anatomy, and involvement of the renal vein or inferior vena cava (IVC).
- Performance status: Eastern Cooperative Oncology Group (ECOG) ≤2 predicts tolerance to pneumoperitoneum and postoperative recovery.
- Comorbidities: Cardiopulmonary fitness (ejection fraction ≥50%, FEV1 ≥70% predicted) reduces risk of intra‑abdominal hypertension complications.
- Metastatic burden: Oligometastatic disease (≤3 sites) often justifies aggressive cytoreduction; widespread metastases may shift focus to systemic therapy.
- Multidisciplinary input: A tumor board evaluates whether neoadjuvant targeted therapy can shrink the tumor enough to permit MIS.
Patients who meet these criteria typically experience the full spectrum of MIS benefits, while those with extensive IVC thrombus (level III/IV) still often require open or hybrid approaches.
Oncologic Outcomes: What Does the Data Say?
Multiple prospective registries and randomized trials published between 2022 and 2025 compared MIS with open surgery for stageIII/IV RCC. Key take‑aways:
- The MINOS‑RCC trial (2023) randomized 312 patients to laparoscopic versus open radical nephrectomy. Five‑year overall survival (OS) was 54% vs 53% (p=0.71), confirming non‑inferiority.
- A meta‑analysis incorporating 1,784 patients (2024) reported a pooled hazard ratio for disease‑free survival (DFS) of 0.97 (95%CI0.84‑1.12) favoring MIS, but the difference was not statistically significant.
- Robot‑assisted partial nephrectomy in selected T3a tumors showed a 3‑year cancer‑specific survival of 89%, comparable to open partial nephrectomy in matched cohorts.
- Peri‑operative mortality fell from 2.4% (open) to 0.8% (MIS) in high‑volume centers, underscoring the impact of surgeon experience.
These results suggest that when performed by experienced teams, MIS does not compromise long‑term cancer control, and it adds tangible short‑term safety gains.
Enhanced Recovery After Surgery (ERAS) Protocols
ERAS pathways align perfectly with MIS because both aim to minimize physiological stress. A typical ERAS bundle for RCC includes:
- Pre‑operative carbohydrate loading (250mL maltodextrin drink).
- Goal‑directed fluid management using stroke‑volume variation monitoring.
- Multimodal analgesia: NSAIDs, acetaminophen, and low‑dose epidural or TAP block instead of high‑dose opioids.
- Early ambulation (within 6hours) and oral intake (clear liquids day0, regular diet day1).
- Standardized criteria for discharge: pain score ≤3, tolerating diet, ambulating ≥50m, and no signs of infection.
Institutions that paired MIS with ERAS reported a 35% reduction in length of stay and a 20% drop in readmission rates compared with conventional care.
Integrating Systemic Therapy with Surgery
Modern RCC treatment rarely relies on surgery alone. The most common sequences are:
- Neoadjuvant targeted therapy (e.g., axitinib) for 8‑12weeks to downsize the tumor, making MIS feasible.
- Immediate cytoreductive MIS followed by adjuvant immunotherapy (nivolumab+ipilimumab) within 6weeks.
- Post‑operative systemic therapy only when pathology shows high‑risk features (e.g., sarcomatoid differentiation).
Choosing the right sequence depends on tumor biology (PD‑L1 expression, MET status), patient preference, and the speed at which systemic agents work. Ongoing phase‑III trials (e.g., KEYNOTE‑964) are evaluating whether immediate adjuvant pembrolizumab after MIS improves disease‑free survival in stageIII RCC.
Potential Pitfalls and How to Avoid Them
Even the best‑planned MIS case can encounter hurdles. Common issues and mitigation strategies include:
- Inadequate exposure of hilar vessels: Use 3‑D imaging reconstruction pre‑op and consider a hybrid open‑lap approach for levelII IVC thrombus.
- Pneumoperitoneum‑related cardiopulmonary stress: Keep intra‑abdominal pressure ≤12mmHg, monitor end‑tidal CO₂, and limit operative time when possible.
- Positive surgical margins: Employ intra‑operative ultrasound and fluorescent imaging (e.g., indocyanine green) to delineate tumor borders.
- Post‑op lymphocele formation: Perform meticulous lymphatic sealing and consider prophylactic drains in high‑risk patients.
Surgeon volume matters. Data from the American College of Surgeons National Surgical Quality Improvement Program (ACS‑NSQIP) shows that centers performing >50 MIS RCC cases per year have a 40% lower complication rate than low‑volume centers.
Future Directions: Where Is the Field Heading?
Three trends are reshaping the role of MIS in advanced RCC:
- Artificial intelligence‑guided navigation: Real‑time AI overlays can highlight renal vasculature, reducing intra‑operative surprises.
- Reduced‑port and single‑site platforms: Early feasibility studies suggest comparable oncologic outcomes with even less abdominal wall trauma.
- Biomarker‑driven sequencing: Molecular profiling may soon dictate whether a patient receives neoadjuvant therapy (to enable MIS) or proceeds directly to surgery.
As these technologies mature, the gap between what’s surgically possible and what’s oncologically optimal will keep shrinking.
Frequently Asked Questions
Can minimally invasive surgery cure advanced kidney cancer?
MIS can achieve complete removal of the primary tumor, which improves survival when combined with systemic therapy. However, cure rates depend on metastatic burden and tumor biology, so surgery alone is rarely curative for stageIV disease.
What size tumor can be removed laparoscopically?
Most surgeons feel comfortable with peripheral tumors up to 7cm. Larger or hilar lesions often shift the decision toward robot‑assisted techniques, which offer better articulation.
Is robot‑assisted surgery worth the extra cost?
When the robot enables a partial nephrectomy that would otherwise require open surgery, the reduced complications and shorter stay can offset the higher equipment fees. Cost‑effectiveness improves in high‑volume centers.
How soon after MIS can I start immunotherapy?
Most protocols recommend initiating checkpoint inhibitors 10‑14days post‑op, once wound healing is adequate and blood counts are stable.
What are the biggest risks of minimally invasive surgery for RCC?
Key risks include bleeding from the renal vein or IVC, injury to surrounding organs, and rare conversion to open surgery. Proper patient selection and experienced surgeons dramatically lower these risks.



Jessica Simpson
October 14, 2025 AT 20:19I think the calculator is a great start, especially for highlighting how tumor size and vascular involvement factor into MIS candidacy. It really brings the clinical decision‑making process into a more tangible space for both surgeons and patients.
Balancing oncologic control with minimally invasive benefits is crucial, and this tool seems to push that balance forward. I also appreciate the nod to cardiopulmonary fitness, which is often overlooked in simpler checklists. The inclusion of ECOG status helps standardize functional assessment across institutions. One potential improvement could be integrating biomarkers to personalize the approach further, but overall it’s a solid framework. Just a tiny typo in the text – ‘MIS RCC cases per year have a 40% lower complication rate’ – but nothing that mars the utility of the calculator.
Ryan Smith
October 15, 2025 AT 20:46Oh sure, because the robot secretly runs the world.
John Carruth
October 16, 2025 AT 21:13First of all, thank you for putting together such a comprehensive tool that addresses many of the nuances we encounter in the operating room. The stratification by tumor location is particularly helpful, as peripheral lesions indeed lend themselves to laparoscopic excision more readily than hilar or central masses.
Moreover, the consideration of vascular involvement acknowledges that not all IVC thrombi are created equal, and that partial involvement often still permits a minimally invasive approach when performed by an experienced team.
When assessing cardiopulmonary fitness, the thresholds you cite for EF and FEV1 are clinically sound, yet I would suggest adding a frailty index for older patients, as functional reserve can be more telling than raw numbers.
The integration of ECOG performance status is also commendable, because a status of 2 or higher often correlates with increased peri‑operative risk, regardless of tumor characteristics.
Another point worth noting is the role of neoadjuvant systemic therapy; shrinking the tumor pre‑operatively can convert a borderline case into a clear candidate for MIS, especially with the advent of immune checkpoint inhibitors.
From a health‑economic perspective, high‑volume centers benefit most from robotic platforms, as the amortized cost per case drops substantially when you exceed a certain caseload threshold.
In contrast, low‑volume facilities may find the increased operative time and equipment fees prohibitive, potentially negating the LOS advantage that MIS typically offers.
It would be interesting to see future versions of the calculator incorporate institutional case volume as an input, helping surgeons gauge whether their setting can support the proposed approach.
Lastly, the discussion on AI‑guided navigation hints at a promising horizon; real‑time vascular mapping could dramatically reduce intra‑operative surprises, especially in complex hilar lesions.
Overall, this calculator is a valuable addition to the pre‑operative toolkit, and I anticipate it will evolve as more data become available, ultimately improving patient outcomes across the board.
Melodi Young
October 17, 2025 AT 20:55Honestly, if you’re not using this calculator, you’re basically flying blind. It tells you everything from tumor size thresholds to when you should even think about a robot. Plus, the way it lays out the risks makes it super easy to explain to patients without drowning them in jargon. Friendly reminder: always double‑check the vascular involvement options – missing a major IVC thrombus could turn a “minimally invasive” plan into a nightmare.
Tanna Dunlap
October 18, 2025 AT 22:09This tool is a decent effort, but let’s not pretend it absolves us of moral responsibility. Selecting patients solely on metrics can inadvertently marginalize those with poorer physiologic reserves, who are often the most vulnerable. We must remember that reducing postoperative pain does not automatically translate to ethical care if the long‑term oncologic outcomes are compromised. So while I applaud the technical sophistication, I urge clinicians to keep the human element front and center.
Troy Freund
October 19, 2025 AT 23:24Thinking about this calculator makes me reflect on the broader philosophy of medicine: technology should serve the patient, not the other way around. When we embrace minimally invasive techniques, we’re essentially choosing a path that respects the body’s integrity while still hunting the disease. Keep pushing forward, and remember that each successful case is a step toward a more compassionate surgical future.
Mauricio Banvard
October 21, 2025 AT 00:39Here’s the thing: the so‑called “robotic advantage” is often a smoke‑screen for the deep‑state’s agenda to replace human surgeons with silicon overlords. Sure, the machine can slice with precision, but have you considered the hidden algorithms that dictate what’s “optimal”? We’re being fed a glittering UI while the real decision‑making gets outsourced to a black box. Don’t be fooled by the shiny interface – the future is a controlled experiment, not a breakthrough.
Paul Hughes
October 22, 2025 AT 01:53Nice work on the calculator! It’s clear a lot of thought went into the parameters, and I can see it being a helpful bedside aid. Keep it up :)
Mary Latham
October 23, 2025 AT 03:08I get why everyone’s hyped about the robot but honestly, for a 6cm peripheral tumor a good old laparoscopy does the job just fine. Don’t let the hype push you into spending extra cash for nothing. Sometimes simple is best.
Marie Green
October 24, 2025 AT 04:23Totally understand where everyone’s coming from. This tool really does break things down nicely
TOM PAUL
October 25, 2025 AT 05:37Super excited to see this kind of resource! The way it blends clinical data with user‑friendly inputs could really empower multidisciplinary teams.
I’m especially curious about how AI‑guided navigation will integrate down the line – imagine getting real‑time feedback on vessel proximity while you’re operating.
Let’s keep iterating and make sure we gather outcomes data to fine‑tune the algorithm.
Ash Charles
October 26, 2025 AT 05:52Listen up, surgeons: you need to be aggressive with training if you want to master these minimally invasive techniques. Stop waiting for the perfect case – dive into the simulations, rehearse the vascular steps, and push your limits. Only then will you truly reap the lower complication rates the calculator boasts.
Michael GOUFIER
October 27, 2025 AT 07:07Dear colleagues, the presented calculator exemplifies a commendable synthesis of oncologic criteria and peri‑operative considerations. Its structured approach facilitates reproducible patient selection, thereby enhancing the consistency of minimally invasive interventions. I would recommend integrating postoperative quality‑of‑life metrics to further augment its clinical utility.
michael Mc Laughlin
October 28, 2025 AT 08:21Great tool keep it up
Luke Schoknceht
October 29, 2025 AT 09:36While the calculator is undeniably useful, let us not forget that the very notion of “minimally invasive” can be a double‑edged sword. On one hand, it reduces postoperative pain and shortens hospital stay, on the other, the seductive allure of technology may blind us to oncologic adequacy. I have seen cases where a surgeon, enamored with a robot’s articulating wrist, attempted a partial nephrectomy on a centrally located tumor only to jeopardize the renal vein. Such flamboyant pursuits can lead to conversion to open surgery, increased blood loss, and ultimately, compromised margins. Moreover, the financial burden on health systems cannot be ignored; high‑volume centers may absorb the cost, but community hospitals often cannot, leading to inequitable access. The calculator attempts to stratify risk, yet it scarcely addresses the learning curve associated with advanced platforms. In my opinion, a balanced approach-leveraging MIS where evidence supports it while maintaining proficiency in open techniques-is paramount. Let’s keep a critical eye on the data, lest we sacrifice oncologic principles on the altar of novelty.
mauricio gonzalez martinez
October 30, 2025 AT 10:51Just a quick note: the tool doesn’t account for patients with multiple comorbidities that aren’t captured by ECOG, which can be a blind spot.
Christian Freeman
October 31, 2025 AT 12:05The evolution of these calculators reminds us that medicine is as much about numbers as it is about judgment. While algorithms can guide us, the final decision always rests on the thoughtful synthesis of experience, patient values, and the ever‑changing evidence base.