Probiotic & Antibiotics Calculator
Calculate Your Probiotic Strategy
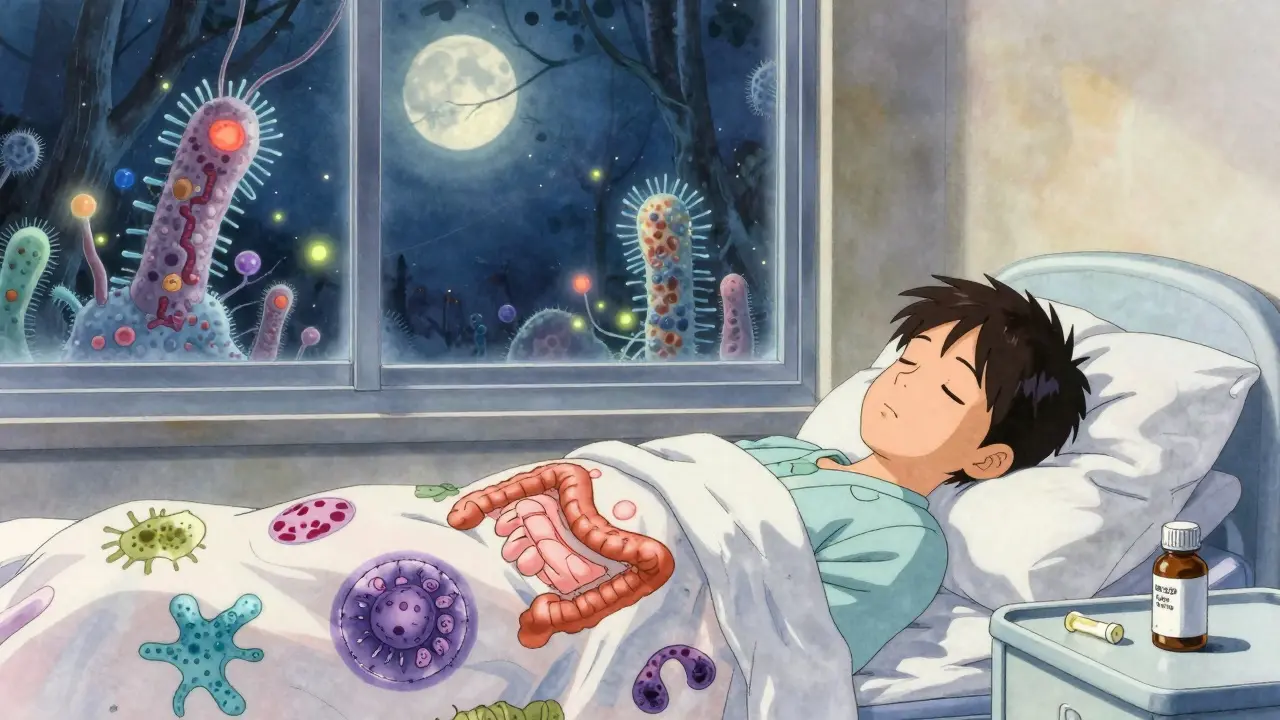
When you’re on antibiotics, you know the drill: take the pills, feel better, but then… the stomach cramps, the bloating, the diarrhea. It’s not just annoying - it’s common. Up to 30% of people on antibiotics get antibiotic-associated diarrhea (AAD), and for some, it’s worse: Clostridioides difficile infection, a dangerous gut bug that can turn a simple course of meds into a hospital stay. That’s where probiotics come in. Not as a magic cure, but as a real, science-backed tool to help your gut survive the antibiotic storm.
Why Your Gut Gets Hit Hard by Antibiotics
Antibiotics don’t just kill the bad bacteria. They wipe out the good ones too. Your gut is home to trillions of microbes - bacteria, yeasts, fungi - that help digest food, train your immune system, and keep harmful bugs in check. When you take an antibiotic like amoxicillin or clindamycin, it doesn’t discriminate. It kills pathogens, but also strips away Lactobacillus, Bifidobacterium, and other friendly residents. This imbalance lets opportunistic pathogens like C. diff move in. The result? Diarrhea, gas, nausea, and sometimes serious illness.Probiotics Can Cut Diarrhea Risk by Over Half
The good news? Taking probiotics while on antibiotics can cut your risk of diarrhea by 42% to 66%. That’s not a guess - it’s from over 8,600 patients in clinical trials. Two strains stand out: Lactobacillus rhamnosus GG and Saccharomyces boulardii CNCM I-745. These aren’t just any probiotics. They’re the ones studied the most, with the strongest evidence.L. rhamnosus GG works by sticking to the gut lining and blocking harmful bacteria. S. boulardii is a yeast, not a bacteria, which means antibiotics don’t kill it. That’s why it’s often preferred for broad-spectrum antibiotics like piperacillin-tazobactam. Both have been shown in multiple studies to reduce the duration and severity of diarrhea.
A 2022 review of 29 studies found that patients taking these strains had a 66% lower chance of getting C. diff. That’s huge. For someone on a long antibiotic course - say, two weeks for pneumonia - this could mean the difference between staying home and ending up in the hospital.
Not All Probiotics Are Created Equal
You can’t just grab any bottle labeled "probiotic" off the shelf. The market is flooded with products, and many don’t deliver what they promise. Independent testing by ConsumerLab found that 23% to 45% of probiotic supplements don’t contain the strains or amounts listed on the label. Some have no live bacteria at all.Look for these things:
- Specific strain names - not just "Lactobacillus," but Lactobacillus rhamnosus GG or Saccharomyces boulardii CNCM I-745.
- CFU count - aim for 10 billion to 50 billion colony-forming units per dose. That’s the range shown effective in trials.
- Refrigerated storage - live cultures are fragile. Refrigerated products often have higher survival rates (78% vs. 62% for shelf-stable ones).
- USP Verified - this label means the product was tested for purity and potency. Only 8% of probiotics have it, but it’s worth paying extra for.
Brands like Culturelle (L. rhamnosus GG) and Florastor (S. boulardii) are the most commonly recommended and widely available. They’re not expensive - typically $20 to $45 for a month’s supply.

When and How to Take Them
Timing matters. If you take your probiotic at the same time as your antibiotic, the antibiotic might kill the good bacteria before they can do their job. The best practice? Take the probiotic 1 to 2 hours after your antibiotic dose. That gives the antibiotic time to work and the probiotic time to settle in.Start on day one of your antibiotic treatment. Don’t wait until you feel sick. Probiotics need time to colonize. Most studies show protective effects kick in after 48 hours. Keep taking them for the full length of your antibiotic course - and then for another 1 to 2 weeks after you finish. This helps your gut microbiome bounce back faster.
One Reddit user, u/MedStudent2023, wrote: "Taking Culturelle with my 10-day amoxicillin course completely prevented the diarrhea I’ve had with previous antibiotics." That’s the kind of real-world result you’re aiming for.
The Risks: When Probiotics Can Backfire
Probiotics are generally safe. Most side effects are mild - a little gas or bloating for the first few days. About 8.7% of users report this, and it usually goes away.But there are serious risks for a small group:
- Immunocompromised patients - people on chemotherapy, with HIV, or after organ transplants. There are documented cases of probiotic bacteria entering the bloodstream and causing infection. Between 2010 and 2020, 12 such cases were reported. If you’re immunocompromised, talk to your doctor before taking anything.
- Central lines or severe pancreatitis - the FDA warns against probiotics in these cases. The risk of infection is too high.
- Antibiotic resistance genes - a 2025 study found that 38% of commercial probiotics carry genes that make bacteria resistant to antibiotics like tetracycline and macrolides. The FDA is now requiring screening for these genes. It’s a new concern, but not a reason to avoid probiotics entirely - just choose reputable brands with verified labels.
What the Experts Really Think
There’s debate. The Infectious Diseases Society of America (IDSA) says probiotics are a good idea for high-risk patients. The American Gastroenterological Association (AGA) says no - because product quality is so inconsistent. But here’s the key point: both sides agree that specific strains like L. rhamnosus GG and S. boulardii work.Dr. Elisa Marroquin, lead author of a major 2022 review, put it simply: "When participants take antibiotics, we see several consistent changes in bacterial species. But when treatment was combined with probiotics, the majority of those changes were less pronounced and some changes were completely prevented."
Most doctors in the U.S. - 62% - recommend probiotics for AAD. But only 28% do it routinely. Why? Insurance doesn’t cover it. Hospitals don’t stock it. It’s not part of the standard protocol. But that doesn’t mean it doesn’t work.
What About Fecal Transplants?
Fecal microbiota transplantation (FMT) is more effective than probiotics for preventing recurrent C. diff - about 37% more effective. But FMT is invasive, expensive, and carries higher risks. It’s used for severe, recurring cases, not routine prevention.Probiotics are the first line. They’re safe, cheap, and easy. If you’re on antibiotics for a simple infection - strep throat, sinusitis, UTI - probiotics are your best bet. FMT is for the rare cases where everything else fails.
What If Probiotics Don’t Work for You?
Some people still get diarrhea even with probiotics. That’s not your fault. Not every strain works for every person. If you tried one and it didn’t help, try a different one. Switch from L. rhamnosus GG to S. boulardii. Or try a multi-strain product that includes Bifidobacterium strains - newer research shows they help restore gut balance after antibiotics.Also, check your timing. Are you taking the probiotic at the same time as your antibiotic? That’s the #1 mistake. Separate them by at least 2 hours. And make sure you’re taking enough - 10 billion CFUs or more.
And if you’re still having issues? Talk to your doctor. You might need a different antibiotic, or you might have an underlying condition. Don’t assume it’s just "your gut being sensitive."
Looking Ahead: The Future of Probiotics
The probiotic market is growing fast - worth over $56 billion in 2022. But the next wave isn’t just random blends. Researchers are developing precision probiotics - defined mixtures of specific strains designed to target certain antibiotic effects. One, called VE303, showed a 76% reduction in C. diff in early trials. These won’t be available over the counter for a few years, but they’re coming.Regulation is catching up too. The FDA’s new draft rules will require probiotic makers to test for antibiotic resistance genes. That means better, safer products. In the next 3 to 5 years, you’ll see fewer sketchy bottles and more science-backed options.
For now, stick with the proven strains. Take them correctly. And know that you’re not just preventing diarrhea - you’re helping your gut heal faster. That’s worth the few extra dollars and the extra step of timing your pills right.
Can I take probiotics at the same time as my antibiotic?
It’s not recommended. Antibiotics can kill the probiotic bacteria before they have a chance to work. Take your probiotic 1 to 2 hours after your antibiotic dose. This gives the antibiotic time to act and the probiotic time to settle into your gut.
Which probiotic strain is best for reducing antibiotic diarrhea?
The two best-studied strains are Lactobacillus rhamnosus GG and Saccharomyces boulardii CNCM I-745. Both have strong clinical evidence showing they reduce the risk of antibiotic-associated diarrhea by 42% to 66%. Look for these exact names on the label.
How long should I take probiotics after finishing antibiotics?
Continue taking probiotics for 1 to 2 weeks after your antibiotic course ends. This helps your gut microbiome recover more fully. Stopping too soon can leave you vulnerable to lingering imbalances.
Are probiotics safe for everyone?
Most people can take them safely. But if you’re immunocompromised - such as from chemotherapy, HIV, or an organ transplant - probiotics can cause serious infections. Avoid them unless your doctor approves. Also avoid them if you have a central line or severe pancreatitis.
Do probiotics help with all types of antibiotics?
They’re most effective with common antibiotics like amoxicillin, clindamycin, and ciprofloxacin. Their benefit is less clear with broad-spectrum antibiotics used in hospitals, like piperacillin-tazobactam. But even then, Saccharomyces boulardii still shows protection against C. diff.
Can probiotics cause antibiotic resistance?
Some commercial probiotics carry genes that make bacteria resistant to antibiotics like tetracycline and macrolides. A 2025 study found this in 38% of products. The FDA is now requiring manufacturers to screen for these genes. Choose USP Verified products to reduce this risk.
Is it worth spending more on a higher-priced probiotic?
Yes, if it means getting a verified product with the right strain and dose. Cheaper brands often have low viability or incorrect labeling. Spending $30 on a USP Verified product with L. rhamnosus GG is better than $15 on a mystery blend. You’re protecting your gut - it’s worth the investment.



Yatendra S
December 16, 2025 AT 14:54kevin moranga
December 17, 2025 AT 14:21Webster Bull
December 19, 2025 AT 01:38Tommy Watson
December 19, 2025 AT 16:53Karen Mccullouch
December 20, 2025 AT 18:19Michael Gardner
December 21, 2025 AT 11:37Willie Onst
December 22, 2025 AT 11:13Ronan Lansbury
December 24, 2025 AT 03:18Constantine Vigderman
December 24, 2025 AT 17:06Casey Mellish
December 25, 2025 AT 23:33Tom Zerkoff
December 26, 2025 AT 08:48