Imagine lying in bed, eyes closed, body still-but your legs won’t stop screaming at you to move. It’s not cramps. It’s not pins and needles. It’s a deep, crawling, aching urge that only eases when you stand up, pace, or jerk your limbs. This isn’t restlessness. It’s restless legs syndrome, or RLS, a neurological condition that steals sleep from millions and leaves them exhausted, irritable, and trapped in a cycle no one else can see.
What RLS Really Feels Like
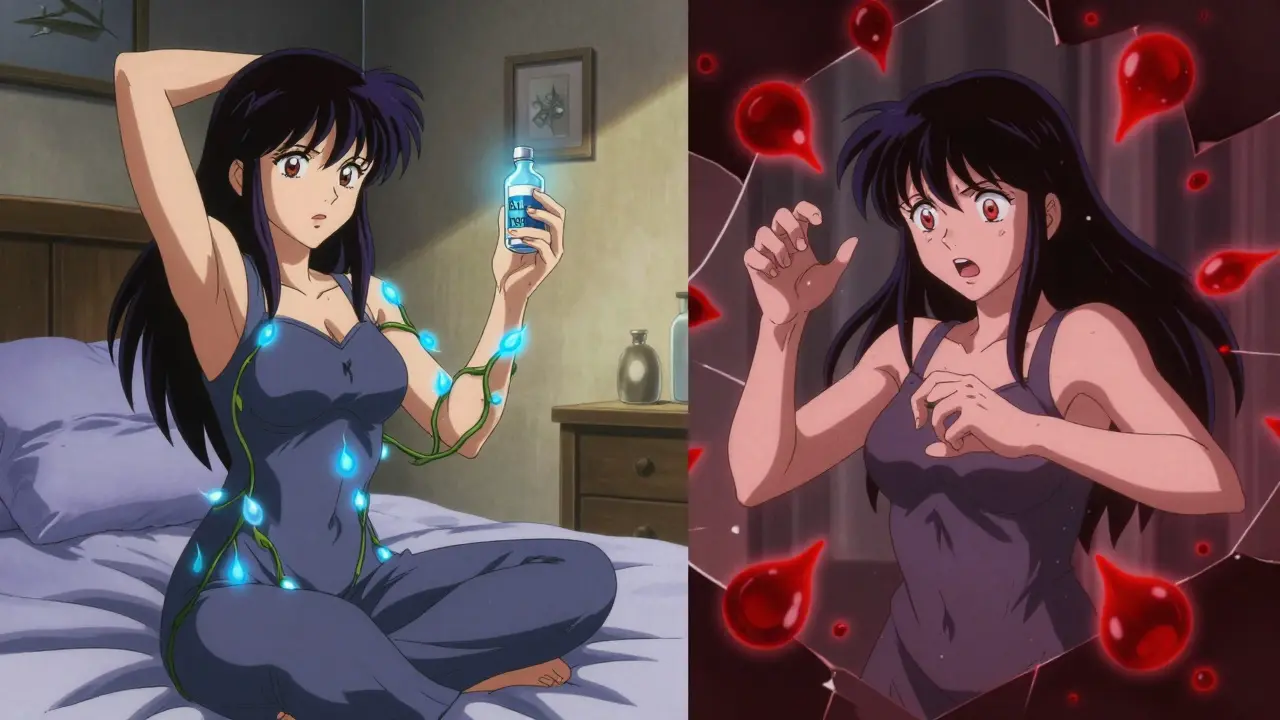
People with RLS don’t just feel fidgety. They feel something wrong in their legs-like ants crawling under the skin, electric shocks, or deep aches that won’t quit. These sensations hit hardest when they’re still: sitting in a movie theater, waiting at the airport, or trying to fall asleep. And they follow a cruel clock: worse after 8 p.m., peak around midnight, and fade by morning. This isn’t anxiety. It’s not stress. It’s a hardwired neurological glitch.
Up to 10% of U.S. adults have RLS, and nearly 90% of them also experience periodic limb movements while asleep-repetitive jerks every 20 to 40 seconds, 15 to 100 times an hour. These movements don’t wake them up, but they keep them stuck in shallow sleep. Polysomnography studies show RLS patients spend 25-40% more time in light sleep (N1 and N2) and 30-50% less in deep, restorative sleep. The result? Average sleep time drops from 7 hours to 4-5. Many don’t even realize they’re sleep-deprived-they just think they’re ‘always tired.’
Why Your Brain Is the Problem
RLS isn’t caused by bad habits or weak willpower. It’s rooted in your brain’s dopamine system. Dopamine is the chemical that helps your brain control movement and regulate sensation. In RLS, the A11 neurons-tiny clusters in the brainstem that send dopamine signals down to the spinal cord-don’t work right. Brain scans show a 20-30% drop in dopamine transporter density in the striatum of RLS patients compared to healthy people.
Iron plays a key role too. Low iron in the substantia nigra-a region rich in dopamine-producing cells-worsens the problem. About half of RLS patients have low ferritin levels (under 75 ng/mL). That’s not full-blown anemia; it’s brain iron deficiency. Iron helps dopamine work properly. Without enough, the system falters.
Genetics also matter. Variants in the BTBD9 and MEIS1 genes increase risk. If a parent has RLS, you’re 50-70% more likely to develop it. That’s why it often shows up in middle age but can strike as early as childhood.
The Sleep Crisis No One Talks About
RLS doesn’t just keep you awake-it rewires your brain’s ability to recover. Daytime consequences are brutal:
- Epworth Sleepiness Scale scores average 12-14 (normal is 5-7)
- Attention and working memory drop by 20-30%
- Reaction times slow to levels similar to being legally drunk
- Motor vehicle accident risk rises by 2.3 times
One 42-year-old woman told her doctor she’d been ‘driving on autopilot’ for years-until she nearly hit a tree. She didn’t realize her brain was shutting down from chronic sleep loss. Her RLS had been untreated for a decade.
And it’s not just physical. Depression, anxiety, and social isolation are common. People skip family dinners, avoid long car rides, and quit jobs that require sitting. The emotional toll is heavy-and often invisible to doctors who don’t ask the right questions.

Dopaminergic Therapy: The Double-Edged Sword
For decades, dopamine drugs have been the go-to treatment. Three FDA-approved options exist: ropinirole (Requip), pramipexole (Mirapex), and rotigotine (Neupro patch). They work fast-symptoms often ease within an hour. In clinical trials, they cut RLS severity scores by 40-50%.
But here’s the catch: they don’t fix the problem. They mask it. And over time, they make it worse.
Augmentation is the biggest risk. It means symptoms start earlier in the day, spread to arms or torso, and feel more intense. A patient who used to have trouble only at night now feels it at noon. A 2020 study called RESTORE found pramipexole caused augmentation in 66% of patients after three years. Rotigotine was better-26%. But even that’s too high.
Why does this happen? Long-term dopamine agonist use tricks the brain into becoming less responsive. The brain downregulates its own dopamine receptors. The drug that once helped now demands higher doses-and still doesn’t work as well.
Then there’s impulse control disorders. About 6-17% of patients develop compulsive behaviors: gambling, binge shopping, hypersexuality. One 52-year-old woman spent $20,000 on online shopping after starting pramipexole. She didn’t even remember buying half the items. The FDA added black box warnings for these risks in 2016.
What Works Better in the Long Run
Alpha-2-delta ligands-gabapentin enacarbil and pregabalin-are now recommended as first-line for chronic RLS. They don’t touch dopamine. Instead, they calm overactive nerves in the spinal cord.
Here’s the trade-off: they take 2-4 weeks to work. But they cause augmentation in only 5-10% of patients. A 2021 JAMA Neurology trial found pregabalin (300 mg nightly) reduced RLS symptoms just as well as pramipexole-but with a third of the augmentation risk.
Iron therapy is another game-changer-for those who need it. If your ferritin is below 75 ng/mL, an IV infusion of ferric carboxymaltose can cut symptoms by 30-40%. It takes 3-6 months to peak, but the relief lasts. No augmentation. No addiction. Just better brain iron.
And lifestyle? It’s not optional. Regular moderate exercise (walking, cycling) helps. Avoiding caffeine, alcohol, and nicotine is critical. Sleep hygiene-consistent bedtime, cool room, no screens-makes a measurable difference. One patient reduced her pill dose by 50% just by fixing her sleep schedule.
How to Use Dopamine Drugs Safely
If dopamine agonists are necessary-say, for severe, intermittent RLS-there’s a smart way to use them:
- Start low: ropinirole 0.25 mg or pramipexole 0.125 mg, taken 1-3 hours before symptoms begin
- Never exceed max doses: 4 mg ropinirole, 0.5 mg pramipexole
- Track symptoms daily: note time of onset, intensity (0-10 scale), and body parts affected
- Watch for early signs of augmentation: symptoms starting before 5 p.m. or spreading to arms
- Re-evaluate every 3 months: if symptoms worsen or spread, switch to an alpha-2-delta ligand
Studies show 83% of augmentation cases are caught within 3 months using a simple symptom diary. Mayo Clinic found patients who tracked their symptoms had 40% better outcomes than those who didn’t.
The Future: Personalized Medicine and New Hope
There’s progress on the horizon. A new extended-release form of ropinirole (Requip XL) cuts augmentation risk by nearly half compared to the old version. Phase III trials showed 18% augmentation at 12 months versus 31%-a big win.
Drugs like fipamezole (an alpha-2 blocker) and intranasal apomorphine are in trials. Fipamezole reduced augmentation by 35% compared to pramipexole. Intranasal apomorphine gives relief in minutes without flooding the system with dopamine.
And genetics? The RLS Pharmacogenetics Consortium can now predict with 72% accuracy whether a patient will respond well to pramipexole-or be at high risk for augmentation-based on their BTBD9 and MEIS1 genes. Soon, testing could guide first-line treatment instead of trial and error.
What You Should Do Right Now
If you suspect RLS:
- Get your serum ferritin tested-aim for over 75 ng/mL
- Start a symptom diary for 2 weeks: time, intensity, triggers
- Eliminate caffeine and alcohol for 30 days
- Try daily walking or light cycling for 30 minutes
- If symptoms persist, see a sleep specialist-not just a GP
If you’re already on dopamine agonists:
- Don’t increase your dose without a specialist’s approval
- Ask about switching to pregabalin or gabapentin enacarbil
- Discuss iron levels-even if your blood count is normal
- Be honest about mood changes, spending habits, or compulsive behaviors
RLS is not a minor nuisance. It’s a neurological disorder that steals sleep, health, and quality of life. But it’s treatable. And the best treatment isn’t always the fastest one. Sometimes, the safest path is the one that doesn’t burn your brain out trying to fix it.
Is restless legs syndrome the same as periodic limb movement disorder?
No, but they’re closely linked. RLS is the urge to move your legs while awake, caused by uncomfortable sensations. Periodic limb movement disorder (PLMD) is the actual involuntary jerking of limbs during sleep. About 80-90% of people with RLS also have PLMD, but many with PLMD don’t have RLS symptoms while awake. PLMD is diagnosed through sleep studies; RLS is diagnosed by symptoms and history.
Can RLS go away on its own?
Rarely. Primary RLS-where there’s no underlying cause like iron deficiency or kidney disease-is chronic and usually worsens over time. Secondary RLS, triggered by pregnancy, medication, or low iron, can improve when the trigger is removed. But for most adults, RLS is a lifelong condition that needs management, not just waiting for it to vanish.
Are dopamine drugs addictive?
Not in the classic sense like opioids or alcohol. But they can cause physical dependence. Stopping suddenly can lead to rebound symptoms worse than before. And the brain adapts-needing higher doses for the same effect. That’s not addiction, but it’s not safe either. That’s why doctors now avoid long-term use unless absolutely necessary.
Why do symptoms get worse at night?
Your body’s dopamine levels naturally drop in the evening. In RLS, the system is already impaired, so the evening dip pushes it past the threshold where symptoms appear. Iron levels in the brain also follow a circadian rhythm, dipping at night. Combine that with reduced movement during rest, and the brain’s signal for movement becomes overwhelming.
Can I use marijuana or CBD for RLS?
Some patients report relief, but there’s no strong clinical evidence yet. Small studies show mixed results. CBD may help with sleep quality, but it doesn’t target the core dopamine issue. It’s not a substitute for proven treatments. If you’re considering it, talk to your doctor-it can interact with other meds and isn’t regulated for dosage or purity.
How do I know if I’m experiencing augmentation?
Look for three signs: symptoms start earlier in the day (like before 5 p.m.), spread to other body parts (arms, torso), or feel more intense than before-even at the same dose. If you notice any of these after starting a dopamine drug, don’t increase the dose. Contact your doctor immediately. Augmentation is a red flag, not a sign the drug isn’t working hard enough.
Is RLS hereditary?
Yes. If one parent has RLS, your risk is 50-70%. Two genes-BTBD9 and MEIS1-are strongly linked to inherited RLS. These genes affect how dopamine and iron are used in the brain. Genetic testing isn’t routine yet, but if you have a family history and early-onset RLS, it’s likely genetic.
What’s the best non-drug treatment for RLS?
Iron supplementation-if you’re deficient. Getting your ferritin above 75 ng/mL through diet or IV iron can cut symptoms by 30-40%. Other effective non-drug approaches include daily moderate exercise (not intense), avoiding caffeine and alcohol, maintaining a regular sleep schedule, and using compression devices or warm baths before bed. Stretching and massage help too, but they’re temporary fixes.


