ECG: Understanding Heart Electrical Activity and Related Diagnoses
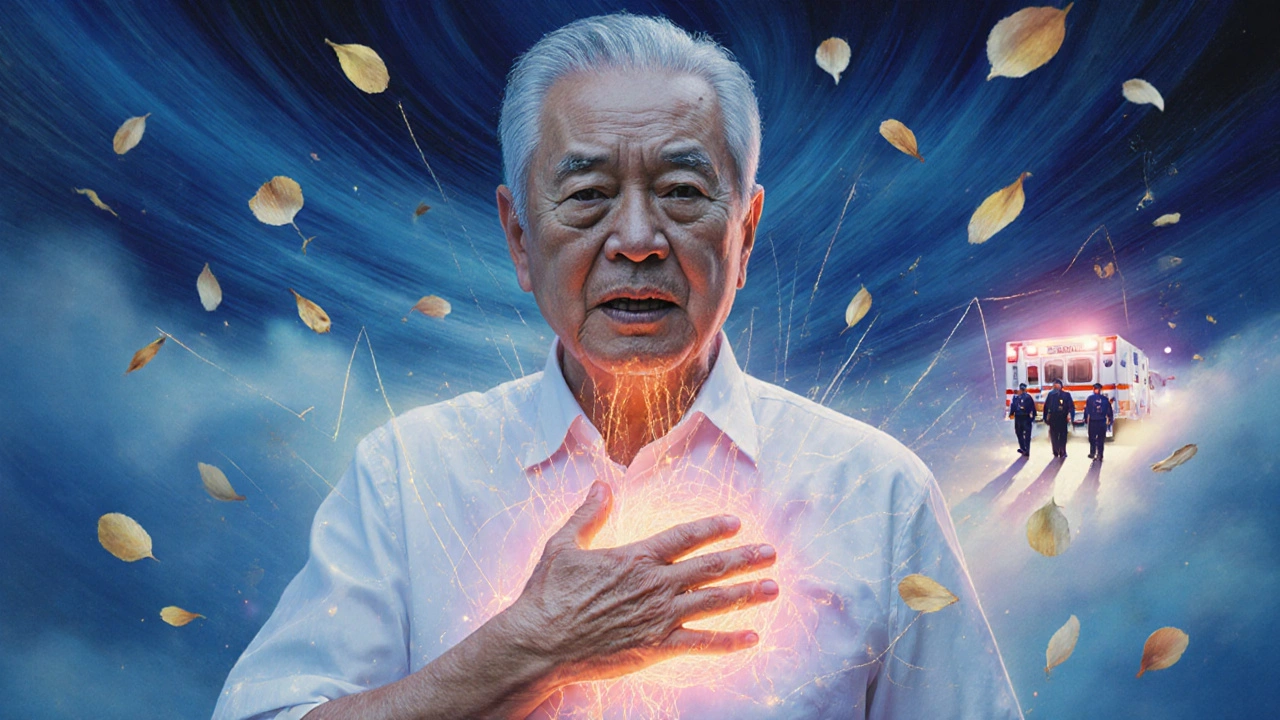
When your heart beats, it sends out tiny electrical signals that control the rhythm. An ECG, a test that records the electrical activity of the heart over time. Also known as electrocardiogram, it’s one of the most common and fastest ways doctors check if your heart is working right. You don’t need to be sick to get one—it’s often done during routine checkups, before surgery, or when you feel dizzy, short of breath, or have chest pain.
ECGs don’t just catch heart attacks. They help spot problems like atrial fibrillation, an irregular and often rapid heart rate that can increase stroke risk, or ventricular hypertrophy, thickening of the heart muscle from high blood pressure or other strain. But they also play a role in diagnosing conditions outside the heart. For example, a sudden drop in oxygen due to a pulmonary embolism, a blood clot in the lungs can show up as abnormal patterns on an ECG—like a fast heart rate or unusual wave shapes. That’s why doctors often order an ECG when someone comes in with unexplained shortness of breath.
What you see on an ECG isn’t just lines—it’s a story. The P wave tells you if the upper chambers are firing right. The QRS complex shows how fast the lower chambers are contracting. The T wave reveals how the heart is recovering after each beat. If any of these look off, it could mean a blocked artery, an electrolyte imbalance, or even side effects from medications like vancomycin or tadalafil. That’s why ECGs are often used alongside other tests like D-dimer or CTPA scans when ruling out serious issues like pulmonary embolism or heart failure.
People with chronic conditions like lupus, diabetes, or COPD often get regular ECGs because their diseases can quietly damage the heart over time. Even if you feel fine, an ECG can catch early signs of trouble before symptoms show up. And if you’re on long-term meds like tamoxifen or rivaroxaban, your doctor might use an ECG to monitor for rare but dangerous changes in heart rhythm.
There’s no magic to it. No needles. No fasting. Just sticky pads on your chest, arms, and legs. You lie still for a few minutes while the machine records your heart’s electrical dance. The results come back fast—often within minutes—and they guide everything from whether you need to go to the ER to whether you should adjust your medication.
What you’ll find below are real-world guides that connect ECGs to the conditions they help diagnose. From how a pulmonary embolism shows up on the readout, to why someone on minocycline or azelastine might need one, to how drug interactions can mess with your heart rhythm—these posts cut through the noise. You won’t find fluff. Just clear, practical info on what an ECG tells you, when it matters, and what to do next.