Emergency Department: What Happens When Things Go Wrong and How Medications Help
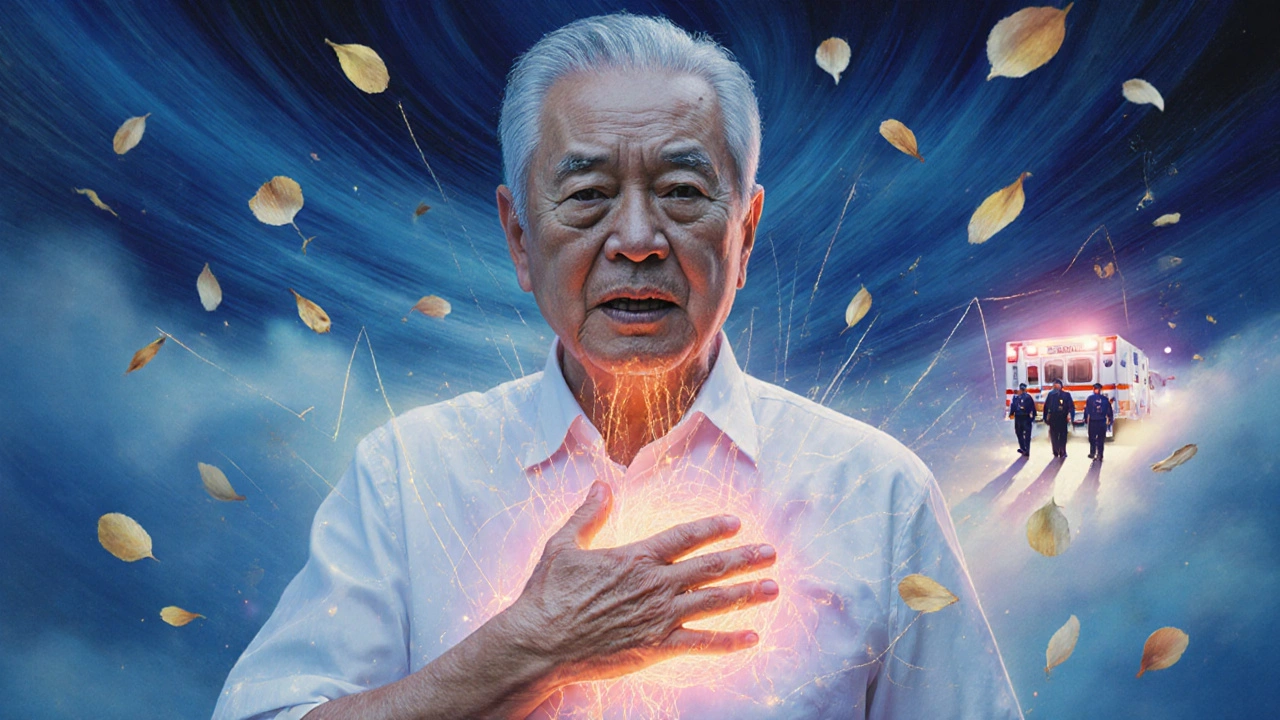
When your body suddenly shuts down—whether from a blood clot, a bad reaction, or a breathing crisis—the emergency department, the frontline of urgent medical care where seconds count and decisions are made under pressure. Also known as the ER, it’s not just a place you go when you’re hurt—it’s where complex drug interactions, life-threatening conditions, and fast-acting treatments collide. This is where a simple cough medicine like guaifenesin might help someone struggling to breathe at night, or where a sudden shortness of breath turns out to be a pulmonary embolism, a deadly blood clot in the lungs that needs immediate imaging and anticoagulants. It’s also where someone on tamoxifen or rivaroxaban might show up with unexpected bleeding or clotting, forcing doctors to untangle their medication history in minutes.
The emergency department, the frontline of urgent medical care where seconds count and decisions are made under pressure doesn’t just treat symptoms—it fights hidden dangers. A patient with lupus might arrive with chest pain, not knowing their immune system has made their blood dangerously sticky, raising the risk of pulmonary embolism, a deadly blood clot in the lungs that needs immediate imaging and anticoagulants. Someone taking tadalafil for erectile dysfunction might collapse after a workout, and the team has to rule out heart strain or dangerous combos with nitrates. Even something as simple as mixing St. John’s wort with an antidepressant can send someone to the ER with serotonin syndrome. These aren’t rare cases—they’re daily realities in the ER, where drug interactions, unexpected and sometimes deadly clashes between medications, supplements, and food are a top concern.
Behind every ER visit is a chain of decisions: Did they take their meds correctly? Is that cough just a cold—or a sign of sleep apnea worsening? Can they afford to wait, or does their D-dimer test need to happen now? The posts here cover the real stories behind those decisions: how CGMs prevent diabetic crashes before they reach the ER, how minocycline clears stubborn skin infections before they turn systemic, how azelastine nasal spray helps people breathe better when pollution spikes, and why checking for drug interactions at home could save you a trip altogether. You’ll find guides on reading prescription labels like BID and PRN, how vancomycin can damage kidneys or hearing if not monitored, and why Cushing’s syndrome or rhabdomyosarcoma might need emergency intervention. This isn’t just a list of articles—it’s a map of what happens when health goes sideways, and how the right knowledge, timing, and meds can turn chaos into control.