Safe Statins with HIV Meds: What You Need to Know
When you’re managing HIV medications, drugs like antiretrovirals that keep the virus under control. Also known as ART (antiretroviral therapy), these drugs are life-saving—but they don’t play nice with everything else in your medicine cabinet. Many people on HIV treatment also need statins, cholesterol-lowering pills that reduce heart disease risk. Also known as HMG-CoA reductase inhibitors, they’re common, but not all are safe to mix with HIV drugs. The problem? HIV meds often block the same liver enzymes that break down statins. That means statin levels can spike, raising your risk of muscle damage, liver stress, or worse.
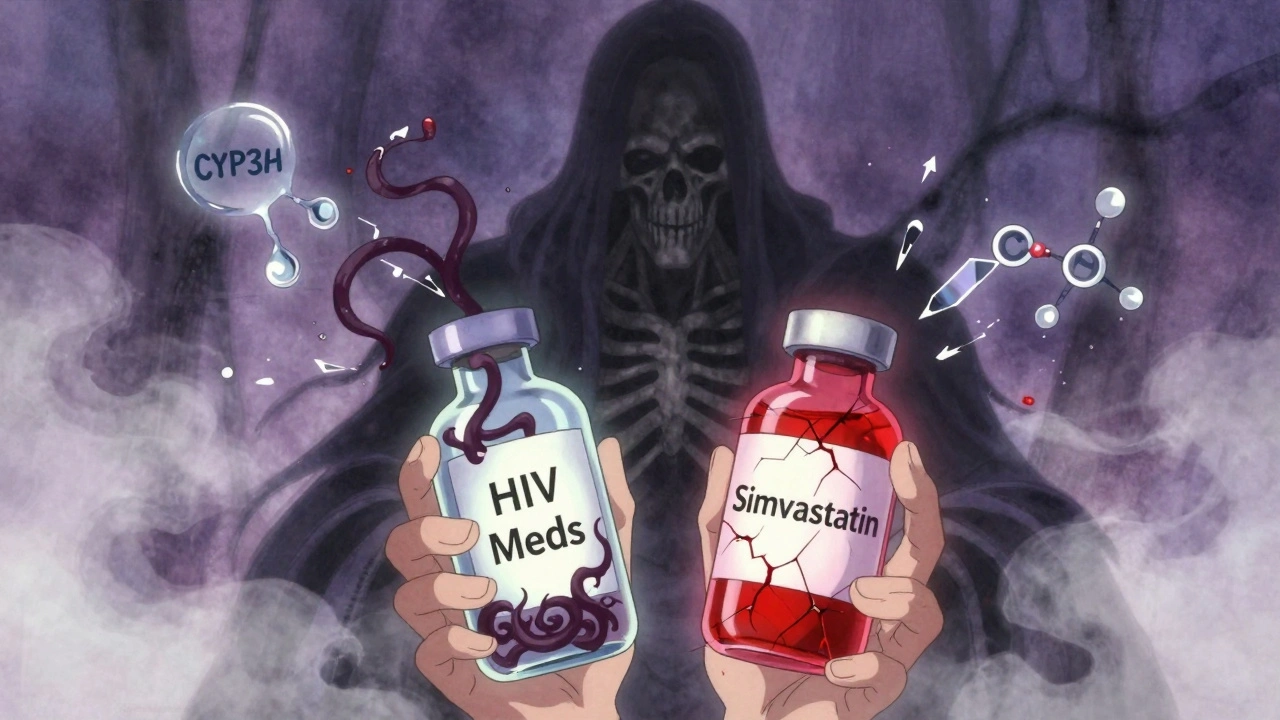
Some statins are safer than others. Pravastatin and rosuvastatin are usually the go-to choices because they’re less dependent on the liver pathways that HIV drugs mess with. Atorvastatin can work too, but only at low doses and with close monitoring. Simvastatin and lovastatin? Avoid them. They’re metabolized by CYP3A4—the exact enzyme boosted or blocked by many HIV drugs like ritonavir and cobicistat. Even a small dose of these two can turn dangerous. It’s not guesswork. Your pharmacist or doctor should check your exact HIV meds before prescribing any statin. This isn’t just about cholesterol—it’s about keeping your liver and muscles healthy while your immune system fights the virus.
It’s not just about the pills. Things like grapefruit juice, certain supplements, or even over-the-counter painkillers can make interactions worse. That’s why so many of the posts here focus on real-world drug clashes—like how grapefruit affects statins, or why caffeine and blood thinners need space. You’re not alone if you’re juggling multiple meds. The key is knowing which combinations are safe, which need tweaks, and how to spot trouble early. Below, you’ll find real, practical advice from people who’ve been there: how to talk to your doctor, what lab tests matter, and how to avoid side effects without giving up your heart health.