When you suddenly see a shower of floaters, or a dark curtain sliding across your vision, it’s not just eye strain. It could be your retina detaching - and retinal detachment is one of the most time-sensitive eye emergencies you can face. If you ignore these signs for even a few hours, you risk permanent vision loss. The good news? If you act fast, surgery can often save your sight. But knowing what to look for - and what to do next - makes all the difference.
What Happens When the Retina Detaches?
Your retina is a thin layer of light-sensitive cells at the back of your eye. It’s like the film in a camera - it captures images and sends them to your brain. When it pulls away from the tissue beneath it, it loses its blood supply and stops working. That’s retinal detachment. Without treatment, the photoreceptor cells start dying within hours. Once they’re gone, they don’t come back. That’s why timing isn’t just important - it’s everything.According to the National Eye Institute, about 1 in 10,000 people experience this each year. But if you’re nearsighted (more than -5.00 diopters), over 40, or had cataract surgery, your risk jumps significantly. A 2022 study in the Beaver Dam Eye Study extension found that people with severe myopia face a risk 167 times higher than the average person.
The Six Emergency Symptoms You Can’t Ignore
You won’t always feel pain, but you’ll notice clear warning signs. Here are the six red flags, backed by clinical data:- Sudden increase in floaters - Not just one or two. Patients describe dozens of new dark spots, squiggles, or cobwebs that appear out of nowhere. The National Eye Institute says this is often the first sign.
- Flashes of light - Like camera flashes in your peripheral vision, especially in dim lighting. These happen when the retina is being tugged by the vitreous gel inside your eye.
- A dark shadow or curtain - This is the most urgent sign. It starts in your peripheral vision and slowly creeps toward the center. NYU Langone Health calls this the clearest indicator that detachment has begun.
- Blurry or distorted vision - If your vision suddenly looks warped, wavy, or out of focus, especially in one eye, don’t wait. Cleveland Clinic data shows this happens in 68% of cases.
- Loss of peripheral vision - You might feel like you’re seeing through a tunnel. The Retina Research Foundation found this occurs in 73% of cases.
- Changes in color perception - Colors may look washed out or dull. This usually means the macula - the part of the retina responsible for sharp central vision - is involved.
One Reddit user, "VisionWarrior22," waited three days after noticing floaters before seeking help. By then, the curtain had spread. Their final vision was 20/100 - far worse than the 20/25 they could have kept with earlier treatment.
How Doctors Diagnose It
If you mention these symptoms to your eye doctor, they’ll start with a dilated fundus exam. This is the gold standard. They’ll use drops to widen your pupil, then look into your eye with a special lens and bright light. It’s not uncomfortable, but it can feel strange.If the view is blocked by cataracts or bleeding, they’ll use B-scan ultrasound - a small probe gently touches your closed eyelid to create an image of the retina. For detailed mapping, they’ll use optical coherence tomography (OCT), which gives a cross-sectional view of the retina like a high-res MRI.
General ophthalmologists miss about 22% of early detachments, according to a 2022 Ophthalmology journal study. That’s why specialists - vitreoretinal surgeons - are the ones who handle these cases. They’ve seen hundreds of them. They know the subtle signs.
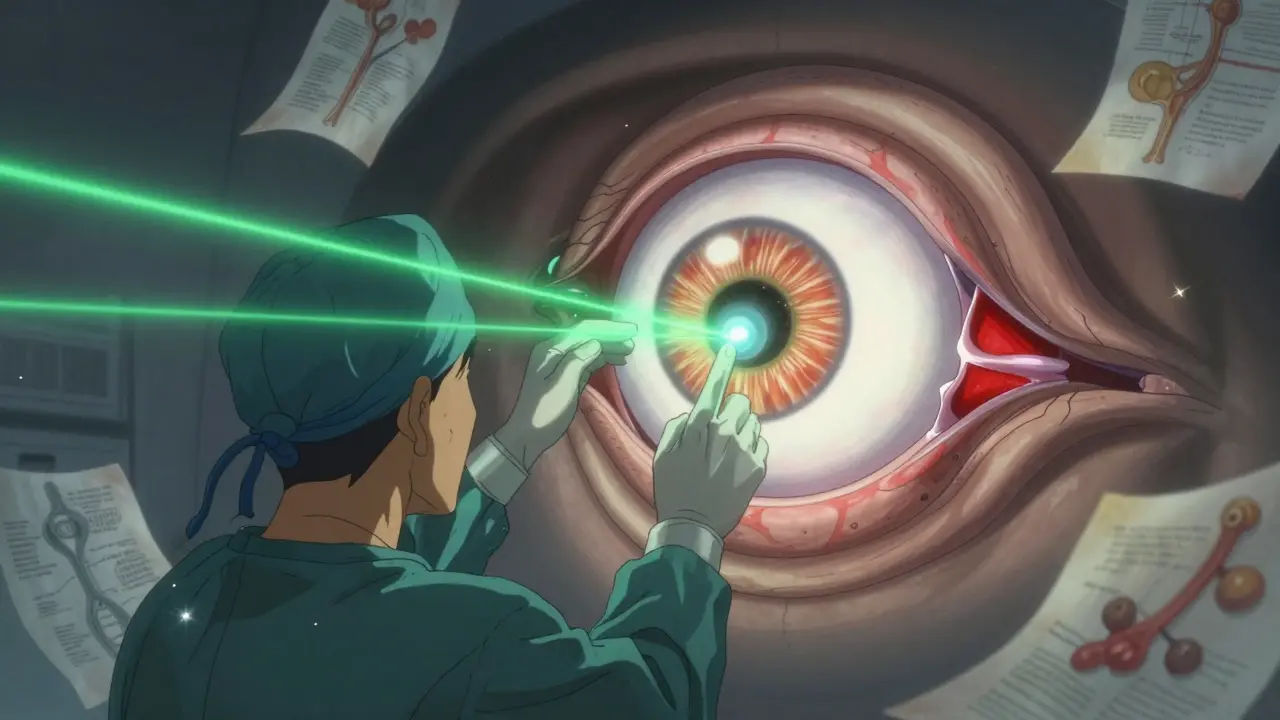
The Three Main Surgical Treatments
There are three primary ways to fix a detached retina. Each has pros, cons, and ideal candidates.Pneumatic Retinopexy
This is the least invasive option. A gas bubble is injected into the eye. You then position your head so the bubble floats up and presses against the detached area. A laser or freezing treatment seals the tear. Success rate? 70-80% for simple, upper retinal breaks. But it only works if the tear is on the top half of the retina. If it’s below, forget it. You’ll need surgery.It’s often used for younger, healthy patients with a single tear. But you’ll need to keep your head in a specific position - face down or turned to one side - for up to 10 days. That’s hard. One patient in the Retina Patient Registry said, "I slept in a recliner for a week. My neck hurt. My back hurt. I couldn’t read or watch TV."
Scleral Buckling
Here, a silicone band is stitched around the outside of your eye. It gently pushes the wall of the eye inward, so the retina can reattach. It’s been used since the 1920s and still works well - 85-90% success for simple cases.But it comes with trade-offs. About 1.5 to 2.0 diopters of nearsightedness is common after surgery. You might need new glasses. There’s also a 5-8% chance of double vision. It’s often chosen for younger patients with lattice degeneration - a condition where the retina has thin, weak spots.
Vitrectomy
This is the most common procedure today. About 65% of all retinal detachments are treated this way. The surgeon removes the vitreous gel (the jelly-like fluid inside your eye) and replaces it with gas or silicone oil. The gas bubble pushes the retina back into place. Laser or freezing seals the tears.Success rate? 90-95%. It’s the go-to for complex cases - like giant retinal tears, advanced scarring, or when the macula is already detached. But there’s a catch: 70% of people who have this surgery and still have their natural lens will develop a cataract within two years. That means another surgery down the line.
A 2022 Cochrane Review found vitrectomy gives better results than scleral buckling when the macula is involved - 92% vs. 85% anatomical success. But if you’re young and want to avoid cataracts, scleral buckling might be better.
Time Is Vision
Dr. Carl Regillo, Chief of Retina at Wills Eye Hospital, says it plainly: "Every hour counts." A 2022 study in the Journal of VitreoRetinal Diseases found that if surgery happens within 24 hours of symptoms, anatomical success jumps to 90%. But if you wait 72 hours? Your chance of regaining 20/40 vision drops from 75% to 35%.That’s why the American Academy of Ophthalmology’s 2023 guidelines say: Same-day evaluation for anyone with symptoms. If the macula is still attached, you have a window. If it’s already detached, time is still critical - but the goal shifts from restoring perfect vision to preventing total blindness.
Wills Eye’s emergency protocol requires a specialist to see you within 4 hours if the macula is off. Surgery should follow within 12 hours. In rural areas, that’s hard. Only 35% of U.S. counties have a retinal specialist. That’s why knowing the symptoms early matters more than ever.
What Happens After Surgery?
Recovery isn’t quick. If you had a gas bubble, you’ll need to stay face-down for 50% of each day for 7 to 10 days. No lying on your back. No looking up. You’ll need special pillows, a mirror to see your TV, and help with meals. About 41% of patients report significant discomfort from this.You can’t fly for weeks - gas expands at high altitude. You’ll need to avoid heavy lifting, bending over, or straining. Your vision will be blurry for days or weeks. Colors may look off. Light may feel too bright. That’s normal.
Complications? Yes. About 25% get higher eye pressure. 5-15% have a recurrence. And as mentioned, cataracts are almost guaranteed in older patients who had vitrectomy. But these are trade-offs - and most people regain functional vision.

Who’s at Risk?
You might think this only happens to older people. But it doesn’t. High-risk groups include:- People with severe myopia (nearsightedness over -5.00D)
- Those who’ve had cataract surgery (0.5-2% risk)
- Patients with lattice degeneration (1% lifetime risk)
- People with a family history of retinal detachment
- Those who’ve had eye trauma
Even if you’re young, if you’ve had a blow to the eye or sudden, violent motion - like a car accident or a fall - get checked. Retinal tears can develop days later.
What Not to Do
Don’t wait. Don’t assume it’s "just aging." Don’t go to your primary care doctor and say, "I think it’s eye strain." A 2023 survey from the American Society of Cataract and Refractive Surgery found 63% of patients were initially misdiagnosed this way. The average delay? 48 hours. That’s two full days of losing vision.Don’t ignore flashes or floaters. They’re not normal. If you’re over 40 and suddenly see them - especially together - call your eye doctor today. If you can’t get in, go to the ER. They can refer you.
Don’t assume surgery means you’re "cured." You’ll need follow-up visits for months. And if you’re at high risk, you might need regular retinal scans - even if you feel fine.
What’s Next?
New tech is coming. In January 2023, the FDA approved the EVA Platform - a 27-gauge vitrectomy system that’s less invasive and heals faster. Intraoperative OCT, which lets surgeons see the retina in real-time during surgery, is now standard in top clinics. And researchers are testing bioengineered retinal patches and gene therapies that might one day prevent detachment in high-risk people.But for now, the best tool you have is awareness. Know the symptoms. Act fast. Get to a specialist. Your vision isn’t something you can afford to gamble with.
Can retinal detachment fix itself?
No. A detached retina cannot heal on its own. The retina needs to be physically reattached and sealed with surgery or laser treatment. Without intervention, the photoreceptor cells die permanently, leading to irreversible vision loss. Even if symptoms seem to improve, the detachment is still present and worsening.
How long after symptoms can surgery still help?
Surgery can still be effective even after several days, but outcomes decline rapidly. If the macula (central vision area) is still attached, surgery within 24 hours gives the best chance of full recovery. If the macula is detached, surgery within 72 hours still has a good chance of preserving functional vision. After 7 days, the success rate drops significantly, and permanent vision loss becomes much more likely.
Is retinal detachment surgery painful?
The surgery itself is not painful. It’s done under local or general anesthesia. Afterward, there may be mild discomfort, pressure, or a scratchy feeling - similar to having sand in your eye. Most patients manage this with over-the-counter pain relievers. Severe pain is rare and should be reported immediately, as it could signal a complication.
Can I drive after retinal detachment surgery?
No, not immediately. You’ll need to wait until your vision clears and your doctor gives approval - usually after 1 to 4 weeks. If gas was used, you can’t fly or drive at high altitudes for several weeks. Always follow your surgeon’s specific instructions. Driving with blurred or uneven vision is dangerous and illegal in most places.
Will I need glasses after surgery?
Possibly. Scleral buckling often changes the shape of the eye, causing new nearsightedness. Vitrectomy can accelerate cataract formation, which also changes your prescription. Most patients need updated glasses within a few months after surgery. Some may eventually need cataract surgery, especially if they’re over 50.
Can I prevent retinal detachment?
You can’t always prevent it, but you can reduce risk. If you’re severely nearsighted, have regular retinal exams every 6 to 12 months. Avoid high-impact sports or activities with a high risk of eye trauma. If you’ve had cataract surgery, report any new floaters or flashes immediately. For people with lattice degeneration, some doctors recommend preventive laser treatment - but this is debated and should be discussed with a retinal specialist.


