Myxedema coma isn’t just a rare complication of hypothyroidism-it’s a ticking time bomb. When thyroid hormone levels crash, the body doesn’t just slow down. It starts shutting down. Breathing gets shallow. Heart rate drops. Body temperature plummets. And the mind? It drifts into confusion, then silence. This isn’t a slow decline. It’s a medical emergency that kills 1 in 3 people if not treated fast. And here’s the scary part: many patients are missed for months, even years, because their symptoms look like depression, dementia, or just getting older.
What Really Happens in Myxedema Coma?
Myxedema coma used to be defined by coma. Now, doctors call it myxedema crisis-because you don’t need to be unconscious to be in danger. The core problem is simple: your body has almost no thyroid hormone left. That means your metabolism, temperature control, heart function, and brain activity all go into free fall. The classic signs? Lethargy so deep you can’t be roused, a body temperature under 35°C (95°F), and a precipitating event like infection, cold exposure, or stopping thyroid meds.
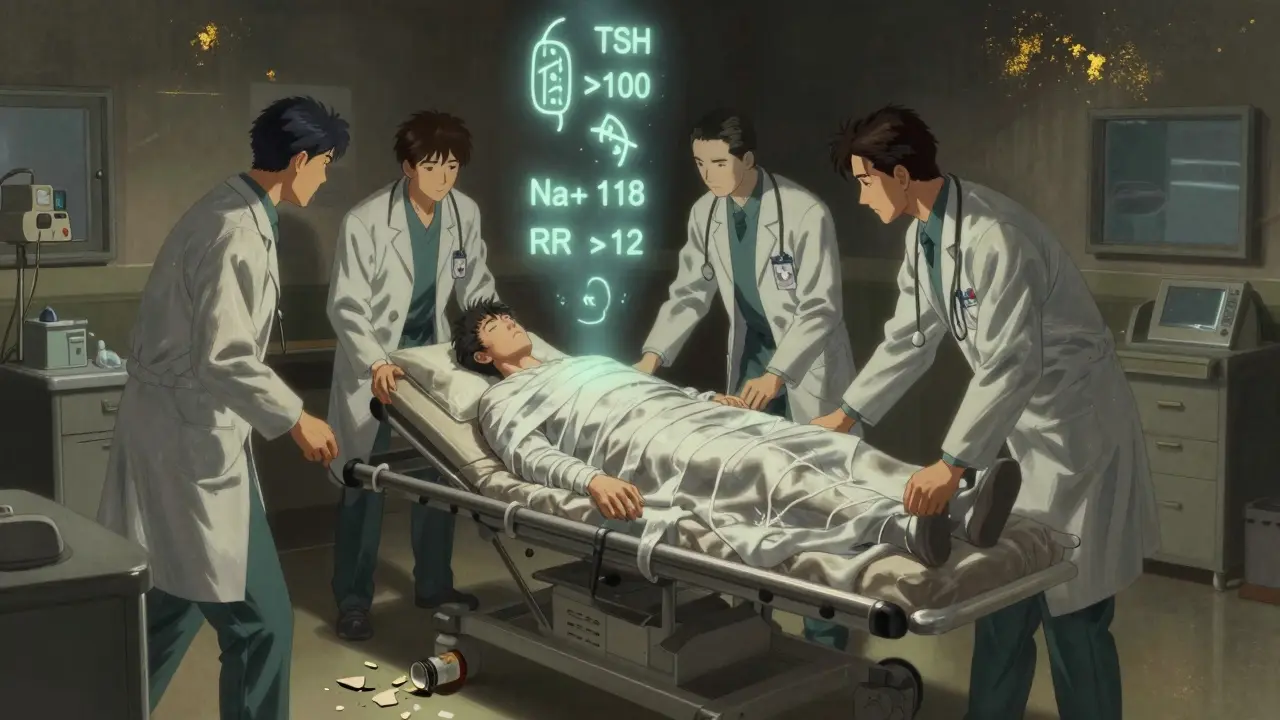
Look at the numbers: 98% of cases show extreme fatigue. 80-90% have dangerous hypothermia. Heart rates often dip below 60 beats per minute. Breathing slows to fewer than 12 breaths per minute. Blood tests? Almost always show low sodium (hyponatremia), high TSH (sometimes over 100 mIU/L), and free T4 levels below 0.9 ng/dL. But here’s the trap: these numbers take hours to come back. Waiting for them is deadly.
Who’s at Risk? It’s Not Just Older Women
Yes, most cases are in women over 60. The ratio is 3:1 female to male. But that doesn’t mean men are safe. In fact, men take longer to get diagnosed-40% of delays happen in male patients. Why? Because doctors don’t expect it. A 55-year-old man with fatigue and cold intolerance? He’s told to drink more coffee. A 70-year-old woman with confusion and constipation? She’s labeled as ‘just aging.’
Winter is the worst time. Cold exposure triggers the crisis in up to 28% of cases. And it’s not just outdoor cold. A poorly heated home, a hospital room turned down too low, or skipping thyroid meds during a hospital stay can be enough. One patient on a thyroid support forum shared: ‘I was admitted for pneumonia, stopped my levothyroxine for ‘safety,’ and woke up in the ICU 3 days later. I didn’t even know I’d stopped taking it.’
How It’s Different From Other Emergencies
Thyroid storm? That’s the hyperthyroid version-racing heart, fever, agitation. Myxedema coma is the opposite: slow, cold, quiet. Diabetic ketoacidosis has clear numbers: high glucose, low pH, low bicarbonate. Myxedema coma? No single lab value confirms it. That’s why clinical judgment is everything.
Think about this: if someone has unexplained low sodium, bradycardia, and altered mental status in winter-especially if they have a history of thyroid disease-don’t wait for labs. Start treatment. The American Thyroid Association says it plainly: ‘Treatment must not wait for laboratory confirmation.’
The Emergency Protocol: What Doctors Do When Seconds Count
There’s a clear, step-by-step approach now. It’s called the DIMES mnemonic: Drugs (medication non-adherence), Infection (most common trigger-pneumonia, UTIs), Myocardial infarction or CVA, Exposure to cold, Stroke. Find the trigger. Treat it. Now.
Here’s what happens in the ER:
- Airway first. Half to 70% of patients need intubation. Their breathing is too weak. Don’t wait for respiratory arrest.
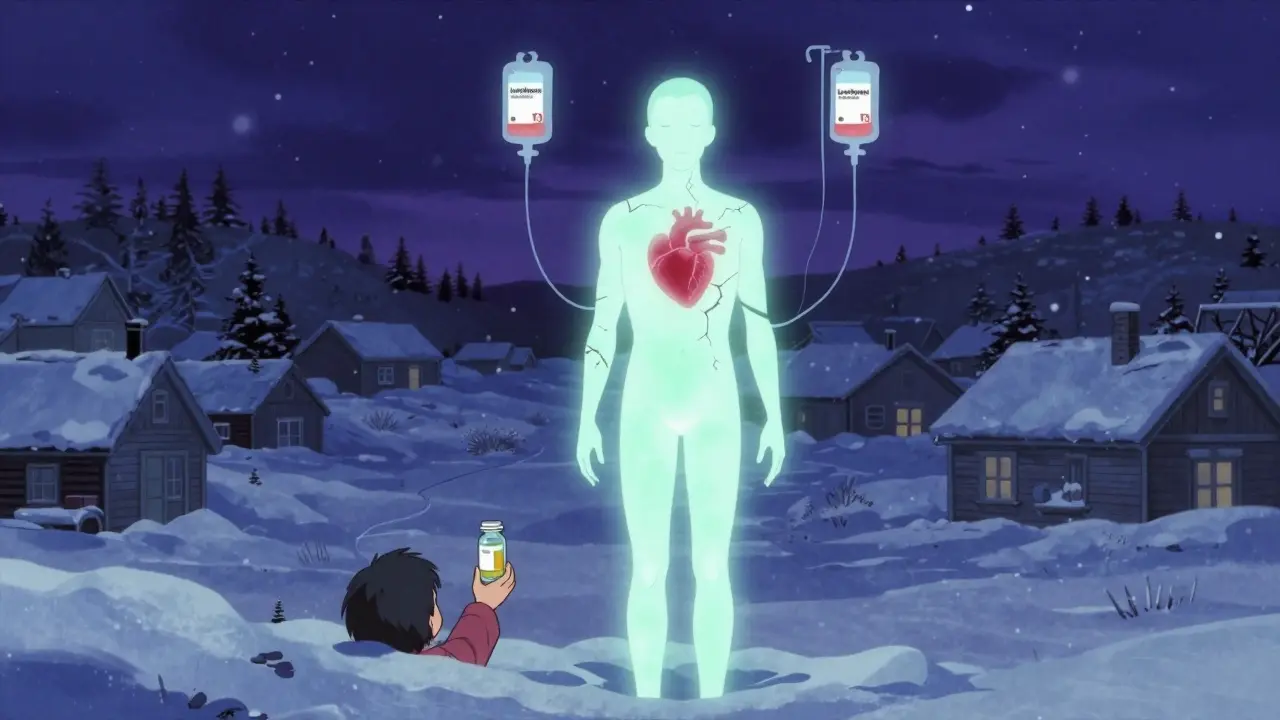
- Thyroid hormone immediately. Give IV levothyroxine (T4) at 300-500 mcg as a loading dose. Then 50-100 mcg daily. For severe cases, especially with heart problems, add liothyronine (T3) at 10-20 mcg every 8 hours. The 2022 Endocrine Society update says T3 is now first-line in critical cases-it works faster.
- Passive rewarming only. No heating blankets, no warm IV fluids. Active warming can shock the heart. Cover them, keep the room warm, monitor core temperature every 30 minutes.
- Treat the trigger. If infection is suspected-even if no fever-start broad-spectrum antibiotics. Pneumonia and UTIs are behind 30-50% of cases.
- Correct sodium slowly. Hyponatremia is common. But correcting it too fast can cause brain damage. Limit sodium rise to 4-6 mmol/L in 24 hours.
Time is brutal here. For every hour treatment is delayed, mortality rises by 10%. Patients treated within 2 hours have survival rates over 70%. Those waiting 12 hours? Survival drops below 40%.
Why Do So Many People Die?
It’s not the disease. It’s the delay.
One 2020 study in the New England Journal of Medicine found uninsured patients waited 35% longer for treatment and had 22% higher death rates. Why? They’re less likely to have regular thyroid checks. They’re less likely to have a doctor who listens.
And then there’s the ‘medical gaslighting’ problem. A 32-year-old man with fatigue, weight gain, and cold intolerance was told he was ‘just stressed’ for 18 months. By the time he collapsed, his TSH was 140 mIU/L. He spent 17 days in ICU. He’s alive now-but he still has brain fog.
Patients who survive often describe the same thing: ‘It felt like I was underwater. Everything was muffled. I couldn’t think.’ That’s not depression. That’s your brain starving for thyroid hormone.
What’s New in 2026?
Two big changes have changed survival rates:
- IV Thyrogen®-a new thyroid hormone formulation approved in January 2023-absorbs faster than older versions. It’s now the standard in trauma centers.
- Point-of-care testing is coming. Devices in phase 3 trials can give TSH and T4 results in 15 minutes with 92% accuracy. Imagine walking into the ER, getting tested, and starting treatment in 20 minutes.
And research is shifting. A 2023 Lancet study found elevated thyrotropin receptor antibodies can predict decompensation before coma hits. That means we might soon be able to prevent it-before it starts.
What You Can Do
If you’re on thyroid medication:
- Never stop it without talking to your doctor-even for a short hospital stay.
- Keep a list of your meds and doses with you. Give it to ER staff if you’re ever admitted.
- Watch for warning signs: extreme fatigue, confusion, cold intolerance, slow heart rate, swelling in your face or legs.
- If you’re over 60, get your TSH checked yearly-even if you feel fine.
If you’re caring for someone with hypothyroidism:
- Don’t dismiss ‘just being tired’ or ‘getting cold easily.’
- If they’re confused or unresponsive, don’t wait. Call 911. Say: ‘I think this might be myxedema crisis.’
- Keep them warm. Avoid cold environments.
Can myxedema coma be prevented?
Yes, in most cases. Regular thyroid function tests, consistent medication use, and avoiding triggers like cold exposure or skipping doses can prevent decompensation. Patients with known hypothyroidism should have TSH checked at least once a year, and more often if they’re elderly, have heart disease, or have had prior episodes.
Is myxedema coma the same as hypothyroidism?
No. Hypothyroidism is a chronic condition where thyroid hormone is low but stable. Myxedema coma is a sudden, life-threatening crash in hormone levels that leads to organ failure. It’s the end-stage of untreated or poorly managed hypothyroidism.
Can you survive myxedema coma without treatment?
Extremely rarely. Without thyroid hormone replacement and supportive care, the body shuts down. Respiratory failure, cardiac arrest, and multi-organ failure are almost certain. Mortality without treatment approaches 100%.
Why is passive rewarming recommended instead of active warming?
Active warming (like heating blankets or warm IV fluids) increases metabolic demand too quickly. The heart and lungs can’t handle the sudden stress when thyroid hormone levels are still too low. This can trigger cardiac arrest. Passive rewarming-using blankets, warm room temperature-lets the body recover slowly as hormone replacement takes effect.
Do all patients need intubation?
No, but nearly half do. Intubation is needed when breathing is too shallow (respiratory rate under 10 breaths per minute), oxygen levels drop below 80 mmHg, or carbon dioxide rises above 45 mmHg. It’s a preventive step-not a last resort. Delaying intubation increases the risk of respiratory arrest.
How long does recovery take after treatment?
Improvement often starts within 24-48 hours of hormone replacement. Mental status improves first, followed by heart rate and temperature. Full recovery can take weeks, especially if there was brain injury from prolonged low oxygen. Most patients return to their baseline thyroid function with continued medication, but some need long-term rehab for neurological effects.
What Comes Next?
The future of myxedema coma isn’t just about better drugs. It’s about better recognition. The growing elderly population means more cases are coming. By 2030, global cases are projected to rise 20%. In places with limited access to thyroid testing, the risk is even higher.
Doctors need training. Emergency rooms need protocols. Patients need to know their own risk. And families? They need to speak up when something feels wrong.
This isn’t a rare disease you’ll never see. It’s a silent killer that hides in plain sight. Know the signs. Trust your gut. And never, ever wait for labs.


