Medicare Part D: What It Covers, How It Works, and What You Need to Know
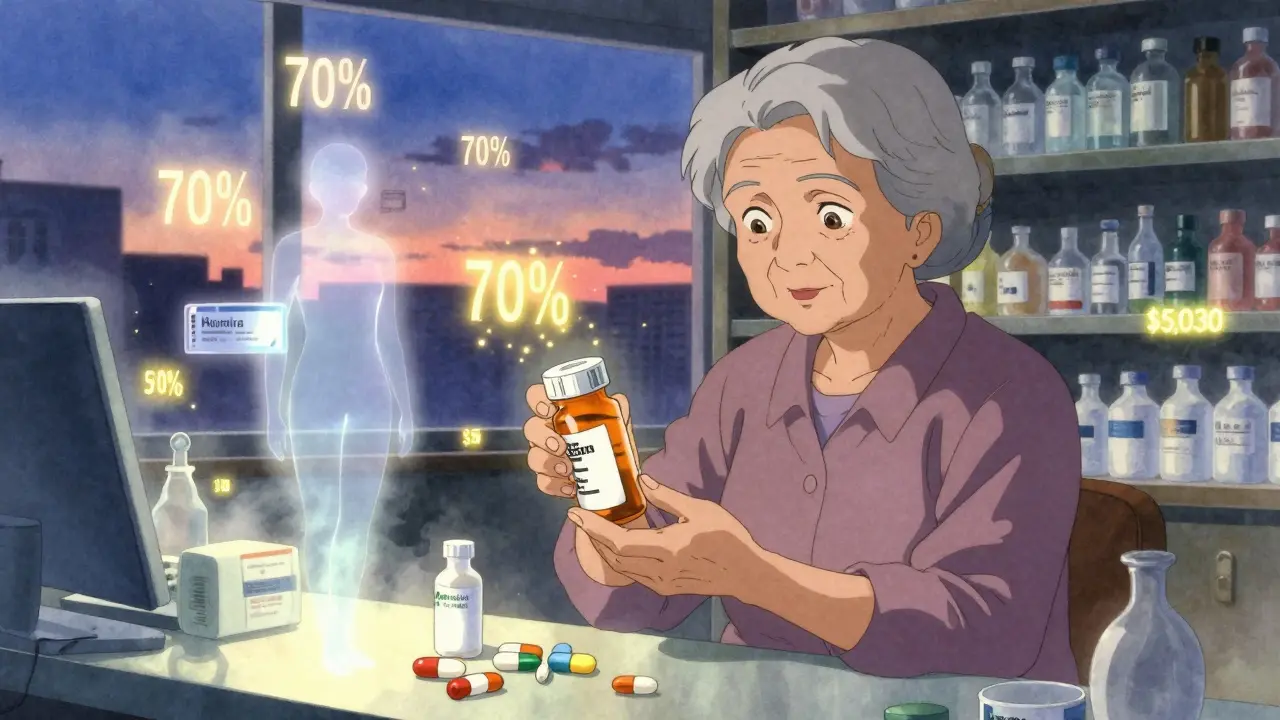
When you’re on Medicare Part D, the federal program that helps pay for prescription drugs for people enrolled in Medicare. Also known as Medicare prescription drug coverage, it’s not automatic—you have to sign up separately, and skipping it can cost you later. If you’re over 65, on disability, or have end-stage renal disease, this is the part of Medicare that keeps your pills affordable. But it’s not one-size-fits-all. Plans vary by cost, which drugs they cover, and where you can fill them.
Medicare Part D works through private insurers approved by Medicare. Each plan has its own formulary, a list of covered drugs, often grouped into tiers with different costs. Some drugs need prior authorization, others require step therapy—you might have to try a cheaper generic first. And if your meds are expensive, you could hit the coverage gap, or "donut hole," where you pay more out of pocket until you hit catastrophic coverage. Low-Income Subsidy, a federal program that helps reduce premiums and copays for people with limited income can ease that burden if you qualify.
It’s not just about picking the cheapest plan. You need to check if your specific meds are covered, what pharmacy network you’re locked into, and whether your doctor’s preferred pharmacy is in-network. A plan that looks cheap might force you to pay more for your daily pills. And if you don’t enroll when you’re first eligible, you might pay a late penalty every month for as long as you have Part D.
People often confuse Part D with Medicare Advantage. But Advantage plans (Part C) bundle Parts A, B, and usually D together. If you’re on Original Medicare (Parts A and B), you need to add Part D separately. And if you’re on Medicaid, you might get drug coverage through both programs—but you still need to pick a Part D plan unless you’re automatically enrolled.
Every year, plans change. Drugs get added or dropped. Prices shift. That’s why open enrollment in October matters—you can switch plans to match your needs for the next year. Don’t wait until you’re out of pills to realize your favorite med isn’t covered anymore.
Below, you’ll find real-world guides on how drug interactions, insurance rules, and pharmacy policies affect your ability to get the meds you need. From how prior authorization delays care to why generic prices vary across states, these posts cut through the noise and show you exactly how Medicare Part D works in practice—not just on paper.