Steroid Taper Calculator
Safe Steroid Taper Calculator
This tool helps you understand the proper tapering schedule for corticosteroids based on your dose and duration of use. Do NOT stop steroids abruptly.
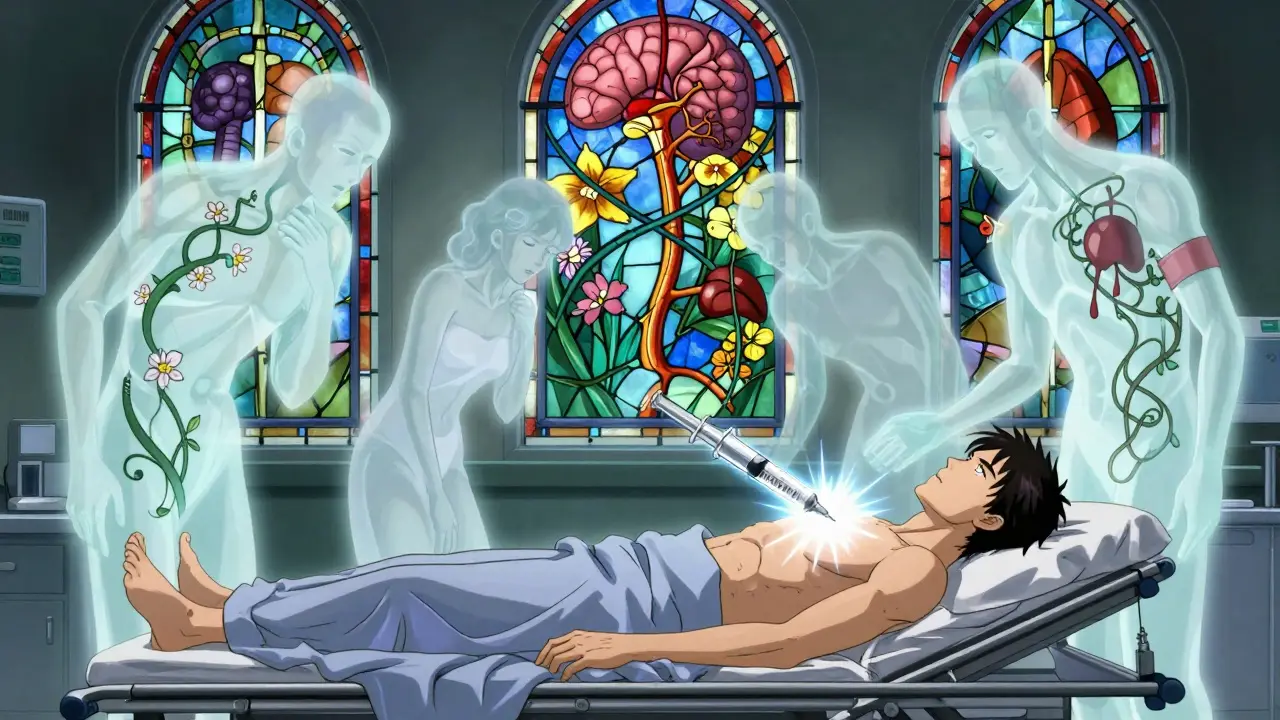
Stopping corticosteroids like prednisone or dexamethasone suddenly can trigger a medical emergency you might never see coming. Even if you’ve only taken them for a few weeks, your body might not be able to make enough cortisol on its own anymore. This isn’t a side effect you can just tough out-it’s adrenal insufficiency, and it can kill you if ignored.
What Happens When You Stop Steroids Too Fast
Your body runs on a delicate balance. The hypothalamus sends signals to the pituitary, which tells your adrenal glands to make cortisol-the hormone that helps you handle stress, keep blood pressure up, and regulate metabolism. When you take synthetic steroids for inflammation, asthma, or autoimmune diseases, your body hears that as "enough cortisol already" and shuts down its own production. Over time, the adrenal glands shrink from disuse. When you stop the pills abruptly, your body has no backup. No cortisol. No emergency response. That’s adrenal insufficiency.It’s not rare. About 1-3% of people in the U.S. are on long-term steroids. And according to the National Institute of Diabetes and Digestive and Kidney Diseases, the most common cause of adrenal insufficiency overall? Stopping steroids too quickly.
Early Signs You Can’t Afford to Ignore
Symptoms don’t show up right away. They creep in 24 to 72 hours after your last dose. At first, they look like the flu, burnout, or depression:- Severe fatigue that doesn’t improve with rest (85% of cases)
- Loss of appetite and unexplained weight loss (72%)
- Nausea, vomiting, or stomach pain (68%)
- Muscle weakness so bad you can’t climb stairs (65%)
- Feeling irritable, anxious, or depressed (58%)
These aren’t "just stress." They’re your body screaming for cortisol. If you’ve been on steroids for more than four weeks and start feeling this way after stopping, don’t wait. Don’t assume it’s a virus. Don’t brush it off as anxiety. Call your doctor or go to the ER.
When It Turns Into an Adrenal Crisis
Left untreated, adrenal insufficiency becomes an adrenal crisis. This is life-threatening. Your blood pressure drops dangerously low. You become dehydrated. Your electrolytes go haywire. You might feel confused, faint, or slip into a coma. Mortality rates hit 6% in hospitalized patients, according to the Cleveland Clinic. And it’s often missed-patients are misdiagnosed with urinary tract infections, food poisoning, or mental health issues.A 2023 case report described a 45-year-old woman who thought she had a UTI after stopping dexamethasone. She ended up in the ER with fever, low blood pressure, and vomiting. Only after her cortisol level was checked did they realize she was in crisis. Within minutes of receiving IV hydrocortisone, she improved. That’s the difference between survival and death.
Tertiary vs. Primary vs. Secondary: What’s the Difference?
Not all adrenal insufficiency is the same. There are three types:- Primary: Your adrenal glands are damaged (like in Addison’s disease).
- Secondary: Your pituitary gland doesn’t make enough ACTH to tell your adrenals to work.
- Tertiary: Your hypothalamus stops making CRH-the signal that starts the whole chain. This is what happens with steroid withdrawal.
Tertiary is the most common type in people coming off steroids. It’s not a broken gland-it’s a silenced system. That’s why testing matters. A simple morning cortisol test can help. If your level is below 5 μg/dL within 24 hours of your last dose, you’re at high risk. Above 10 μg/dL? You’re probably fine.
How to Taper Steroids Safely
There’s no one-size-fits-all taper. But here’s what experts agree on:- If you’ve taken more than 20 mg of prednisone daily for over 3 weeks, you need formal testing before stopping.
- For doses above 20 mg: reduce by 2.5-5 mg every 3-7 days.
- For doses between 5-20 mg: reduce by 1-2.5 mg every 1-2 weeks.
- If you’ve been on steroids for more than 6 months, go even slower-some patients need months to taper.
The European Society of Endocrinology recommends 4-8 weeks for most patients. The Endocrine Society says tailor it to you: your dose, your duration, your health, your symptoms. But here’s the catch: 47% of patients don’t follow their taper plan. They quit early because they feel better, or they’re scared of side effects, or they can’t afford the meds. That’s dangerous.
What You Need to Do Right Now
If you’re on steroids-or just came off them-here’s your action list:- Don’t stop cold. Always taper under medical supervision.
- Know the warning signs. Fatigue, nausea, low blood pressure-don’t ignore them.
- Carry emergency hydrocortisone. If you’ve been on steroids for more than 4 weeks, ask your doctor for an injectable form. Keep it with you at all times.
- Wear medical ID. A bracelet or necklace that says "Adrenal Insufficiency" could save your life if you’re found unconscious.
- Get a written plan. A 2023 Mayo Clinic study found patients with written emergency instructions had 79% better outcomes.

What’s New in 2025
Technology is catching up. In 2024, researchers developed AI tools that can predict adrenal crisis risk with 92% accuracy by analyzing your medical records-meds, lab values, symptoms over time. Point-of-care cortisol tests are in phase 2 trials and could give results in 15 minutes instead of days. That means ERs and clinics might soon be able to diagnose adrenal insufficiency on the spot.Genetics is also playing a role. A 2023 study found seven gene variants linked to slower adrenal recovery. In the future, your doctor might test your DNA to figure out how fast you can safely taper.
But the biggest change? Awareness. Since 2021, the FDA has required all systemic steroid packages to include a warning about adrenal insufficiency. The European Medicines Agency now requires patient alert cards in 28 countries. And in 2024, the American Medical Association added adrenal crisis recognition to its mandatory continuing education list for doctors.
Real Stories, Real Risks
One Reddit user, u/AdrenalWarrior, wrote: "My doctors kept telling me it was just post-viral fatigue for six weeks after stopping prednisone for my asthma. Then I collapsed. I had an adrenal crisis. Now I carry hydrocortisone everywhere. I wish I’d known sooner."That’s the pattern: delayed diagnosis, misdiagnosis, near-death. The average time from first symptom to ER visit? 3.2 weeks. And 68% of patients say their symptoms were blamed on something else.
It doesn’t have to be this way. Education saves lives. If you’re on steroids, know the risks. If you’re a caregiver, know the signs. If you’re a doctor-ask about steroid history every time someone comes in with unexplained fatigue or nausea.
Final Thought: This Isn’t Just About Pills
Steroids are powerful. They can save lives. But they come with a hidden cost: your body’s natural ability to respond to stress. That’s why stopping them isn’t just a medical decision-it’s a survival plan. You can’t just quit. You have to be prepared.Adrenal insufficiency isn’t something you recover from overnight. It takes time, patience, and vigilance. But with the right knowledge, it’s completely preventable. Don’t wait for a crisis to learn the lesson. Learn it now.
Can you get adrenal insufficiency after just a few weeks of steroids?
Yes. While it was once believed that only long-term, high-dose steroid use caused adrenal suppression, research since 2023 shows that even short-term use-less than four weeks-and low doses (under 5 mg prednisone daily) can suppress the hypothalamic-pituitary-adrenal axis. The risk increases with longer duration and higher doses, but no duration is completely safe without proper tapering.
How do I know if I’m having an adrenal crisis?
An adrenal crisis includes severe low blood pressure, confusion, vomiting, abdominal pain, fever, and fainting. It often follows worsening fatigue, nausea, and muscle weakness. If you’ve recently stopped steroids and develop these symptoms, treat it as an emergency. Give yourself an emergency hydrocortisone injection if you have one, then call 911 or go to the ER immediately.
Do I need to carry emergency steroid injections forever?
Not necessarily forever, but until your adrenal glands fully recover-which can take months to over a year. Your doctor will monitor your cortisol levels and may perform an ACTH stimulation test to check recovery. Until then, carry the injection. Many patients who’ve had one crisis are advised to keep it on hand indefinitely because the risk of recurrence is high under physical stress (surgery, infection, trauma).
Can I restart steroids if I feel bad after stopping?
Only under medical supervision. Restarting steroids without guidance can reset your adrenal suppression cycle and make future tapering harder. If you’re having symptoms, contact your doctor. They may adjust your taper, run tests, or temporarily restart a low dose to stabilize you before continuing the reduction.
Are there natural ways to help adrenal recovery?
No. While rest, hydration, and good nutrition support overall health, there are no supplements, herbs, or diets proven to speed up adrenal recovery after steroid withdrawal. Your adrenal glands need time and the right hormonal signals (ACTH) to regain function. Trying to "boost" them with supplements can be misleading and dangerous. Stick to your doctor’s taper plan and avoid unproven remedies.
What if I’m pregnant and need to stop steroids?
Pregnancy doesn’t eliminate the risk of adrenal insufficiency-it may increase it. Cortisol is critical for fetal development, and sudden withdrawal can harm both you and the baby. Tapering must be done under the care of an endocrinologist and obstetrician. Emergency hydrocortisone is safe during pregnancy and should be carried. Never stop steroids abruptly during pregnancy without medical advice.



Jody Patrick
December 17, 2025 AT 01:14Radhika M
December 19, 2025 AT 00:00Philippa Skiadopoulou
December 20, 2025 AT 04:50Pawan Chaudhary
December 21, 2025 AT 16:24Jonathan Morris
December 22, 2025 AT 19:01Linda Caldwell
December 24, 2025 AT 10:28Anna Giakoumakatou
December 24, 2025 AT 23:49CAROL MUTISO
December 25, 2025 AT 01:58Erik J
December 25, 2025 AT 13:14BETH VON KAUFFMANN
December 25, 2025 AT 14:05Martin Spedding
December 27, 2025 AT 02:44Raven C
December 28, 2025 AT 11:33