If you have asthma and find your symptoms get worse every spring, or after cleaning the house, or when your dog jumps on the bed-you’re not alone. About 60% of adults with asthma have allergic asthma, where everyday allergens like pollen, dust mites, or pet dander don’t just cause sneezing-they trigger wheezing, chest tightness, and panic attacks with a rescue inhaler. This isn’t just coincidence. It’s a direct link between your immune system’s overreaction to harmless substances and the chronic inflammation in your airways. Managing asthma isn’t just about inhalers anymore. If allergies are driving your symptoms, you need to treat the root cause, not just the flare-ups.
Why Allergies Make Asthma Worse
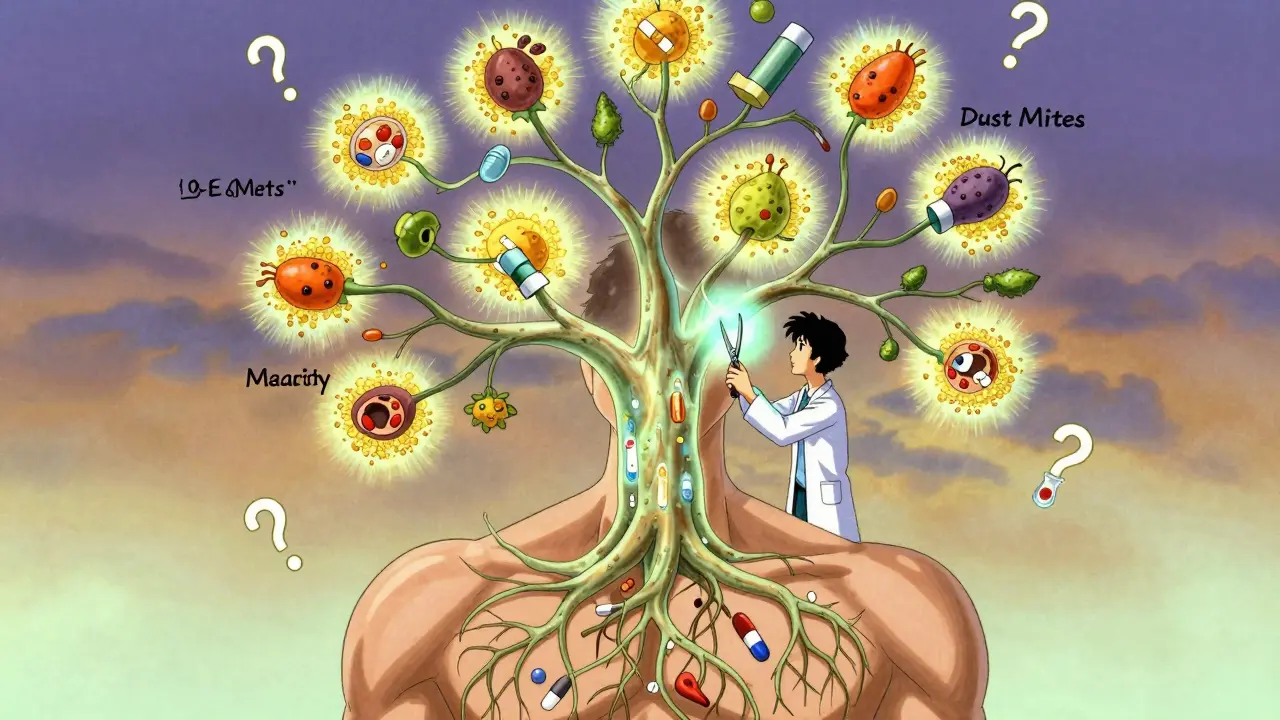
When you breathe in an allergen like cat dander or mold spores, your body treats it like an invader. Immune cells release IgE antibodies, which then activate mast cells in your airways. These cells dump out histamine and other inflammatory chemicals, causing swelling, mucus production, and muscle tightening around your bronchial tubes. That’s asthma. It’s not that allergies cause asthma-most people with allergies don’t get asthma-but when both are present, they feed each other. The same inflammation that gives you a runny nose also narrows your lungs.
This isn’t just theory. Studies show that people with allergic asthma have higher levels of eosinophils-white blood cells that drive chronic airway inflammation-than those with non-allergic asthma. Their airways are literally more inflamed, more sensitive, and more reactive. And it shows in real life: during peak pollen season, emergency room visits for asthma spike by 30-50%. If you’re using your inhaler more than twice a week, or waking up at night with coughing or wheezing, your allergies might be the hidden culprit.
How to Know If Allergies Are Triggering Your Asthma
You can’t guess your triggers. You need proof. The first step is allergy testing. Skin prick tests are still the gold standard. A doctor places tiny drops of common allergens on your arm or back, then lightly pricks the skin. If you’re allergic, a small red bump appears within 15-20 minutes. Blood tests that measure specific IgE levels can also confirm sensitivities, especially if skin testing isn’t safe or available.
But testing alone isn’t enough. You need to connect the dots. Keep a symptom diary for a few weeks. Note when you feel worse: after mowing the lawn? After vacuuming? After your partner brings the dog inside? Did your symptoms start after moving to a new home? Did they get worse after your child got a pet? Correlating exposure with symptoms is the key to identifying your personal triggers.
And don’t assume you’re only allergic to one thing. Most people with allergic asthma react to multiple allergens. Dust mites, pollen from trees and grasses, mold, cockroaches, and pet dander are the top five. If you’re allergic to more than one, managing them all becomes critical.
What Works: Real Strategies to Reduce Airway Inflammation
Once you know your triggers, the goal is simple: reduce exposure and calm the inflammation. But not all strategies are equal.
Allergen avoidance sounds easy, but it’s often poorly done. Buying a HEPA filter won’t help if you still sleep on a dusty mattress. Covering your mattress and pillows with allergen-proof covers reduces dust mite exposure by up to 85%. Wash bedding weekly in hot water (at least 130°F). Remove carpets, especially in bedrooms. Use a vacuum with a HEPA filter-regular vacuums just kick dust back into the air. If you have a pet, keep it out of your bedroom and bathe it weekly. Outside, check daily pollen counts. Apps like Allergy Alert give hyperlocal forecasts, more accurate than national weather reports. On high-pollen days, keep windows closed and shower after coming in.
Inhaled corticosteroids are the backbone of asthma treatment-and they work better in allergic asthma. People with allergic asthma respond to these meds 60-70% of the time, compared to 40-50% in non-allergic cases. But they only work if you take them daily, even when you feel fine. Skipping doses because you’re “not having an attack” is the #1 reason asthma stays uncontrolled.
Allergen immunotherapy is the only treatment that can actually change the course of allergic asthma. It’s not a quick fix-it takes 3-5 years-but it’s the closest thing to a cure. Whether through weekly shots or daily under-the-tongue tablets, immunotherapy trains your immune system to stop overreacting. Cochrane reviews show it cuts asthma symptoms and medication use by 40-60%. One patient in Canberra reduced her rescue inhaler use from four times a week to once a month after two years of dust mite shots. The catch? It’s a long haul. The first few months involve frequent visits and temporary symptom flares. Sixty-five percent of people quit before year two because it feels slow. But if you stick with it, you can cut your long-term medication costs by $1,200 a year.
Biologic therapies are for severe cases. Drugs like omalizumab (Xolair), dupilumab (Dupixent), and tezepelumab (Tezspire) target specific parts of the immune response. Omalizumab blocks IgE, reducing asthma attacks by 50% in clinical trials. Tezepelumab works even in non-allergic asthma, making it a breakthrough. These aren’t cheap-$25,000 to $35,000 a year-but for people who end up in the ER monthly, the cost of hospital stays and missed work often outweighs the price. Insurance usually covers them if you’ve tried at least two other treatments and still aren’t controlled.
What Doesn’t Work (and Why)
Not every “solution” helps. Air purifiers? Helpful only if they’re HEPA-rated and used consistently. Essential oils? No evidence they reduce inflammation-some can even irritate airways. Salt rooms or breathing therapies? No proven benefit for asthma control. And while some people swear by dietary changes like eliminating dairy, studies show no consistent link between diet and asthma severity in allergic asthma. Focus on what the science backs: allergen avoidance, proven meds, and immunotherapy.
Also, don’t ignore non-allergic triggers. Cold air, smoke, exercise, stress, and viral infections can all worsen asthma-even if allergies are the main driver. Managing asthma means managing everything that pushes your airways over the edge.
The Bigger Picture: Why This Matters
Ignoring the allergy-asthma link leads to unnecessary suffering. Dr. Robert Lemanske, former president of the American Academy of Allergy, Asthma & Immunology, says failing to treat allergies is the #1 reason asthma stays out of control. Studies show that 30% of people with poorly controlled asthma have undiagnosed allergies. If your doctor never tested you, you’re flying blind.
And it’s getting worse. The global allergy diagnostics market is growing fast-projected to hit $4.1 billion by 2027. More people are being tested, more biologics are being approved, and integrated health systems like Kaiser Permanente now require allergy testing for uncontrolled asthma patients. The result? A 22% drop in hospitalizations in their network.
But access is unequal. In low-income areas and developing countries, 75% of asthma patients can’t get allergy testing or biologics. Even in places like Australia, out-of-pocket costs for testing can run $250-$400. Insurance doesn’t always cover it. That’s why education is so important. Asthma education programs that teach patients how to manage triggers improve medication adherence by 45% and slash ER visits by 38%.
What to Do Next
If you have asthma and suspect allergies are making it worse, here’s your action plan:
- Track your symptoms for 2-4 weeks. Note timing, location, and possible triggers.
- Ask your doctor for allergy testing-skin prick or blood test. Don’t accept “you probably have allergies” as an answer.
- If tests are positive, start allergen avoidance. Focus on your bedroom first: covers, washing, vacuuming, pet rules.
- Review your asthma meds. Are you taking your inhaled steroid every day? If not, start.
- If you’re still having symptoms despite meds and avoidance, ask about immunotherapy or a referral to a pulmonologist or allergist.
- Consider a FeNO test (fractional exhaled nitric oxide). It measures airway inflammation and helps predict if biologics will work.
There’s no magic bullet. But if you treat the allergic part of your asthma, you’re not just managing symptoms-you’re changing your long-term outlook. Fewer attacks. Less medication. More days without fear. That’s the goal.
Can allergies cause asthma?
No, allergies don’t cause asthma, but they’re the most common trigger for it. About 60% of adults and 80% of children with asthma have allergic asthma, where exposure to allergens like pollen or dust mites directly causes symptoms like wheezing and coughing. The immune response to allergens worsens airway inflammation, making asthma harder to control.
Is allergic asthma different from other types?
Yes. Allergic asthma usually starts in childhood, is linked to eczema or hay fever, and responds better to inhaled corticosteroids. People with allergic asthma have higher levels of eosinophils and IgE, and their symptoms often flare with seasonal allergens. Non-allergic asthma tends to start later in life, isn’t tied to specific triggers, and may respond less predictably to standard treatments.
Do I need allergy testing if I already take asthma meds?
Yes-if your asthma isn’t fully controlled. Even if you’re on daily inhalers, uncontrolled symptoms often mean hidden triggers are still active. Up to 30% of people with poorly controlled asthma have undiagnosed allergies. Testing can reveal what’s making your meds less effective and open up better treatment options like immunotherapy.
How long does allergy immunotherapy take to work?
It’s not fast. Most people start seeing improvements after 6-12 months, but it takes 3-5 years to get full benefit. The first few months involve weekly shots or daily tablets to build up tolerance. Many people quit during this phase because symptoms can temporarily worsen. But those who stick with it often cut their asthma medication in half and have fewer severe attacks long-term.
Are biologics worth the cost?
For severe allergic asthma that doesn’t respond to other treatments, yes. Biologics like omalizumab or dupilumab can reduce asthma attacks by 50% or more. While they cost $25,000-$35,000 a year, they can prevent expensive ER visits, hospital stays, and missed work. Insurance usually approves them if you’ve tried at least two standard treatments and still have frequent flare-ups.
Can I stop my asthma inhaler if I start allergy shots?
Never stop your inhaler without talking to your doctor. Allergy immunotherapy reduces inflammation over time, but it doesn’t work immediately. Many people reduce their inhaler dose after 1-2 years of consistent immunotherapy, but that decision must be made with medical supervision. Stopping too soon can lead to dangerous flare-ups.



gerard najera
December 31, 2025 AT 14:07Allergies don’t cause asthma. They just turn your airways into a warzone. The immune system’s overreach is the real villain-not the pollen, not the dust, not the cat. It’s the misfiring biology. And until we treat the inflammation, not just the symptoms, we’re just rearranging deck chairs on the Titanic.
Phoebe McKenzie
January 2, 2026 AT 07:56Ugh. Another ‘just use a HEPA filter’ post. You think people don’t know this? My mom’s been vacuuming with a HEPA for 12 years and still ends up in the ER every May. The real problem? Big Pharma doesn’t want you to know immunotherapy works-because pills and inhalers are way more profitable. They’re selling you Band-Aids while your lungs rot.
Austin Mac-Anabraba
January 4, 2026 AT 01:02Let’s be precise: allergic asthma is not a comorbidity-it’s a cascade. IgE-mediated mast cell degranulation → eosinophilic infiltration → bronchial hyperresponsiveness → remodeling. This isn’t ‘trigger avoidance’ porn. It’s pathophysiology. And if you’re not measuring FeNO or serum periostin, you’re not managing-you’re guessing. The data is clear: uncontrolled eosinophilic inflammation predicts exacerbations better than FEV1. Stop treating asthma like a seasonal nuisance. It’s a systemic immune dysregulation disorder.
Also, ‘dust mites’? Please. The real culprit is the endotoxin load from gram-negative bacteria in your mattress. Your ‘allergen-proof’ covers are useless if you’re not laundering them in >55°C water weekly. And if you’re using a non-HEPA vacuum? You’re just aerosolizing your own immune trigger.
And immunotherapy? It’s not ‘a long haul.’ It’s the only disease-modifying intervention we have. The Cochrane data is robust. The dropout rate? 65%. That’s not patient laziness-that’s systemic failure. No one tells you about the first 3 months of local reactions, the cost, the time. You get a pamphlet and a ‘good luck.’ No wonder people quit.
Biologics aren’t ‘expensive.’ They’re cost-effective when you factor in ER visits, lost wages, ICU stays. But insurance requires you to fail 2 other treatments first? That’s not clinical-it’s bureaucratic cruelty. And yes, the $30k price tag is obscene-but it’s not the drug’s fault. It’s the patent system’s.
Stop calling it ‘asthma.’ Call it ‘allergic airway inflammation with bronchoconstriction.’ Language matters. If you think ‘avoiding pets’ is a solution, you haven’t read the 2023 JACI meta-analysis on IgE titers and cross-reactivity.
Stephen Gikuma
January 5, 2026 AT 07:31They don’t want you to know this, but the WHO and CDC are hiding the truth: pollen counts are being manipulated to sell more inhalers. The ‘allergy epidemic’? Manufactured. The real cause? Fluoride in the water. It weakens your mast cell membranes. That’s why your body overreacts to dust. And don’t get me started on the 5G towers in your neighborhood-they’re amplifying IgE production. I know a guy in Ohio who stopped using his inhaler after installing a Faraday cage over his bed. He’s been symptom-free for 3 years.
HEPA filters? Useless. They don’t block the nanoscale allergen particles that the government’s been spraying since 2018. You think your ‘dust mites’ are natural? Nah. They’re bioengineered. Look up Project Haywire.
Bobby Collins
January 5, 2026 AT 21:39ok but like… what if your landlord won’t let you remove carpet? and your cat is your emotional support animal? and you’re on a budget? i just want to breathe without crying 😭
Layla Anna
January 7, 2026 AT 08:10Thank you for writing this 💙 I’ve had asthma since I was 5 and just found out last year I’m allergic to dust mites and ragweed… I thought I was just ‘bad at breathing’ 😅 I started washing my sheets weekly and using pillow covers and honestly? I haven’t used my inhaler in 3 weeks. I cried when I realized I could sleep through the night. You’re right-it’s not magic, it’s just… paying attention. 🌿
Donna Peplinskie
January 8, 2026 AT 04:06Oh my goodness, thank you for this post-it’s so rare to see someone actually explain the science without oversimplifying or scaring people. I’ve been on immunotherapy for 18 months now, and yes, the first six months were brutal-itchy, swollen, miserable-but now? I can walk outside without a mask in April. I used to need a rescue inhaler every other day. Now? Once a month. And I’ve saved over $1,800 on meds. It’s not glamorous, but it’s real. If you’re struggling, please don’t give up. Your lungs will thank you. And if your doctor won’t refer you? Find an allergist. You deserve to breathe. ❤️
Olukayode Oguntulu
January 9, 2026 AT 10:44One must interrogate the epistemological framework underpinning this discourse: the conflation of immunological biomarkers with therapeutic agency is a neoliberal reductionism. The IgE-eosinophil axis is not a causal chain but a symptom of a deeper ontological rupture-between the human body and the anthropocene’s chemical substrate. Your HEPA filter? A palliative fetish. Your immunotherapy? A commodified surrender to biopower. The real solution lies not in the clinic, but in the dismantling of industrialized allergen production-i.e., monoculture agriculture, synthetic textiles, and corporate pet food conglomerates. Until we abolish the pet-industrial complex, we are merely rebranding our suffering as ‘management.’
Also, your ‘dust mites’ are just the tip of the iceberg. Have you considered that your mattress is a biofilm of corporate surveillance? The cotton is GMO. The filling is microplastic-laced. Your ‘allergen-proof’ covers? They’re woven with RFID threads. You’re not allergic to dust-you’re allergic to capitalism.