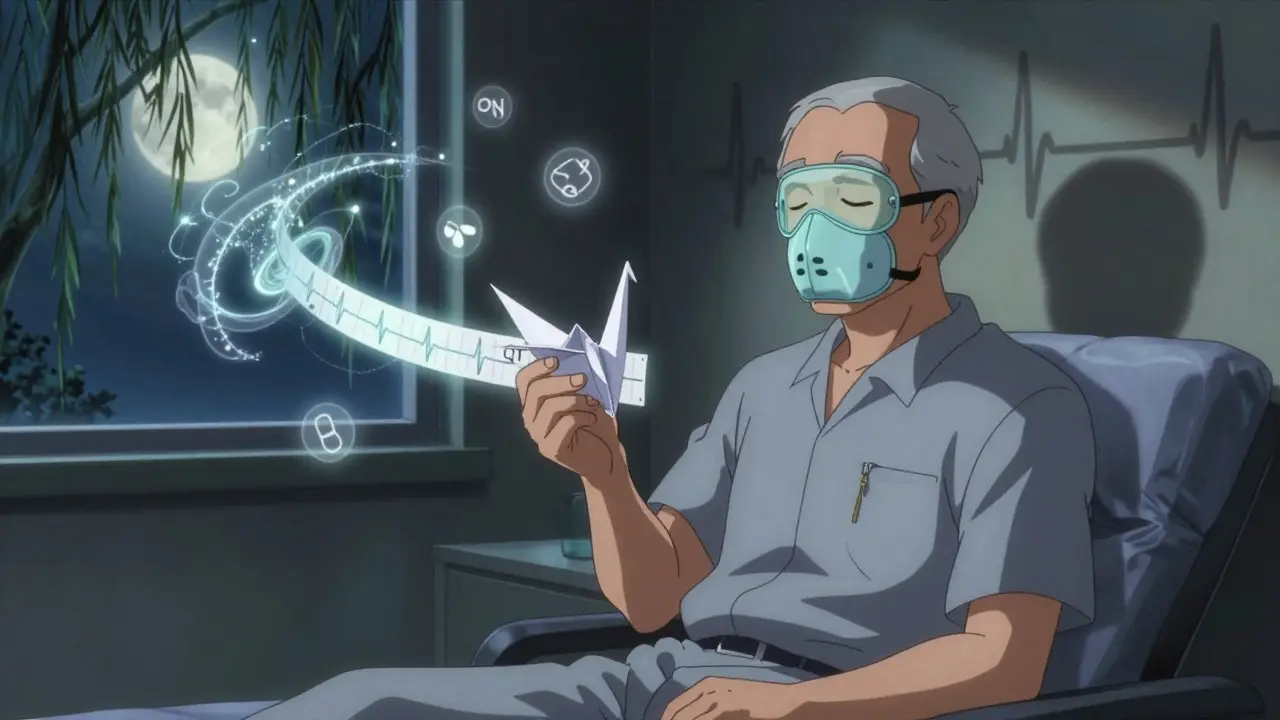
Methadone QT Prolongation Risk Calculator
Methadone QT Prolongation Risk Assessment
Determine your ECG monitoring frequency based on clinical guidelines. This tool helps identify high-risk patients who need more frequent cardiac monitoring.
When someone starts methadone maintenance therapy, the goal is clear: reduce opioid use, lower overdose risk, and rebuild stability. But behind that promise lies a quiet, often overlooked danger - methadone can stretch the heart’s electrical cycle, increasing the chance of a deadly arrhythmia called Torsades de Pointes. This isn’t theoretical. It’s documented, measurable, and preventable - if you know what to look for.
How Methadone Affects the Heart
Methadone blocks a specific potassium channel in heart cells, called hERG (KCNH2). This channel helps reset the heart’s rhythm after each beat. When it’s blocked, the heart takes longer to recharge. That delay shows up on an ECG as a longer QT interval - the time between the start of the Q wave and the end of the T wave.
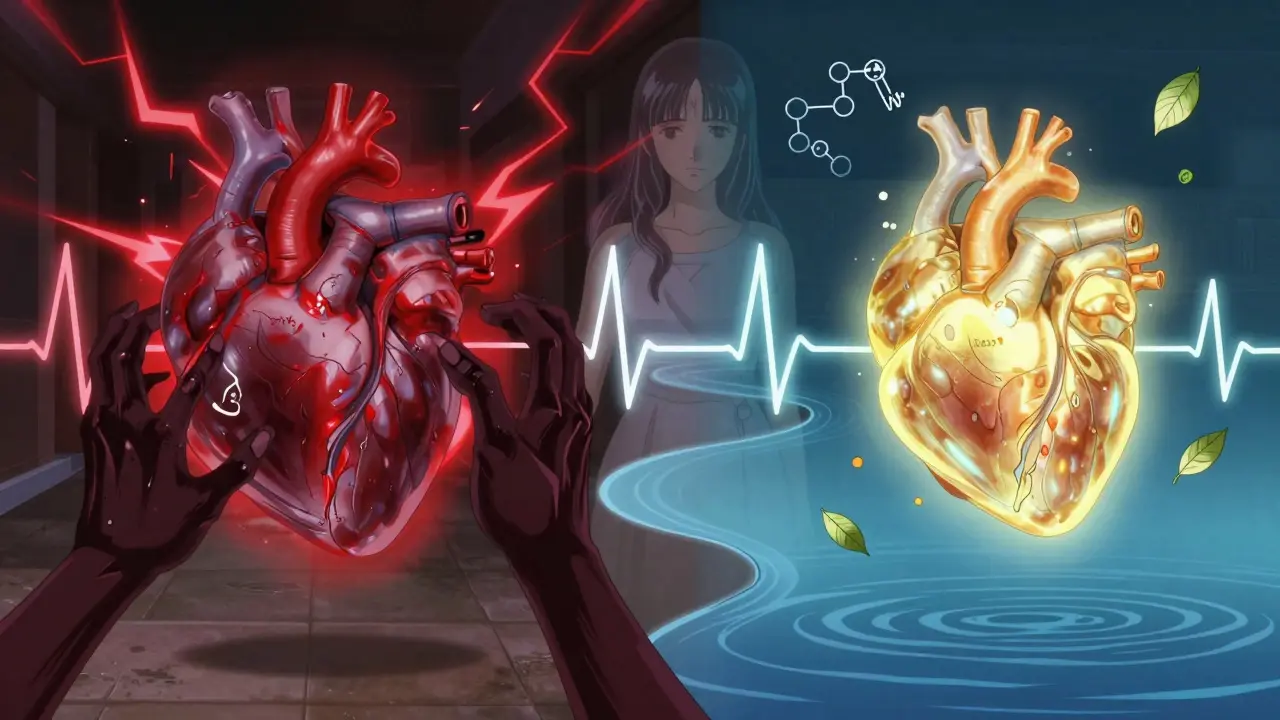
That’s not just a number. A prolonged QT interval means the heart is more vulnerable to chaotic, life-threatening rhythms. The risk spikes when the corrected QT (QTc) goes beyond 450 ms in men or 470 ms in women. At 500 ms or higher, the chance of sudden cardiac death jumps fourfold. And methadone doesn’t just affect one person the same way. Dose matters. Genetics matter. Other drugs matter. Even your potassium level matters.
Who’s at Risk? The Real Risk Factors
Not everyone on methadone needs monthly ECGs. But some people are walking a tightrope. Here’s who’s most at risk:
- Women - They’re 2.5 times more likely than men to develop QT prolongation, even at the same dose.
- People over 65 - Aging slows drug clearance and weakens heart muscle recovery.
- Low potassium or magnesium - Potassium under 3.5 mmol/L or magnesium under 1.5 mg/dL can trigger arrhythmias even with normal QTc.
- Heart disease - Reduced ejection fraction, prior heart attack, or heart failure multiplies risk.
- Other QT-prolonging drugs - Antidepressants like amitriptyline, antipsychotics like haloperidol, or antibiotics like moxifloxacin stack on top of methadone’s effect.
- Drug interactions - Medications that block CYP3A4 enzymes (like fluconazole, voriconazole, or fluvoxamine) can boost methadone blood levels by up to 50%.
- Dose above 100 mg/day - Studies show patients on doses over 100 mg have nearly four times the risk of QT prolongation.
And here’s something rarely discussed: sleep apnea. About half of people on methadone have it. When breathing stops during sleep, oxygen drops. That stresses the heart, making arrhythmias more likely. If someone snores loudly or feels exhausted during the day, that’s not just laziness - it’s a cardiac red flag.
When and How to Monitor: A Clear Protocol
The best approach isn’t “test everyone.” It’s risk-stratified monitoring. Based on current guidelines from SAMHSA and the American Heart Association, here’s what works:
- Baseline ECG before starting - Do it before the first dose. Measure QTc manually, not just relying on machine readings. Machines can be wrong.
- Follow-up at steady state - Wait 2 to 4 weeks after starting or changing dose. Methadone builds up slowly. The real effect shows up after steady state.
- Check electrolytes at the same time - Potassium and magnesium should be in range. If they’re low, fix them before adjusting dose.
After that, frequency depends on risk:
- Low risk - QTc under 450 ms (men) or 470 ms (women), no other risk factors → every 6 months.
- Moderate risk - QTc between 450-480 ms (men) or 470-500 ms (women), or 1-2 risk factors → every 3 months.
- High risk - QTc over 480 ms (men) or 500 ms (women), or 3+ risk factors → monthly ECG. Consider lowering the dose or switching to buprenorphine.
Any QTc increase of more than 60 ms from baseline? That’s a hard stop. Stop increasing the dose. Check electrolytes. Call a cardiologist. Don’t wait.
What to Do If QTc Is Too High
If someone’s QTc hits 500 ms or more, or if they’ve had a sudden spike, don’t panic - but don’t ignore it either.
- Hold dose increases - No more titration until QTc normalizes.
- Correct electrolytes - Give potassium and magnesium if levels are low. Even if they’re borderline, correcting them can prevent events.
- Review all meds - Stop or replace any other QT-prolonging drugs if possible. Antidepressants? Switch to something like sertraline or citalopram (lower risk). Antipsychotics? Consider alternatives.
- Consider buprenorphine - It’s just as effective for opioid dependence, but with far less QT prolongation risk. For high-risk patients, it’s often the safer long-term choice.
- Screen for sleep apnea - If they haven’t been tested, refer them for a sleep study. Treating apnea can reduce arrhythmia risk on its own.
And here’s the truth: many clinics don’t do this well. A 2022 survey of patients on Reddit found 68% had inconsistent ECG monitoring. But those who got regular checks reported 82% confidence in safety - compared to just 47% of those who didn’t. Monitoring isn’t bureaucracy. It’s trust.
The Evidence: Monitoring Saves Lives
A 2023 study in JAMA Internal Medicine looked at methadone clinics that implemented structured QT monitoring versus those that didn’t. The difference? A 67% drop in serious cardiac events. That’s not a small gain. That’s life-or-death.
Between 2000 and 2022, the FDA recorded 142 confirmed cases of Torsades de Pointes linked to methadone. But experts believe that’s a fraction of the real number. Sudden deaths in people with opioid use disorder are often labeled “overdose” - even when the heart stopped first. That’s why routine ECGs matter. You can’t diagnose a silent arrhythmia with a urine test.
And here’s something else: methadone still saves lives. People on maintenance therapy have 33% lower mortality than those who quit. The goal isn’t to stop methadone - it’s to use it safely. That means knowing when to pause, when to check, and when to switch.
Final Takeaway: Don’t Guess. Measure.
Methadone isn’t dangerous because it’s a bad drug. It’s dangerous because we treat it like it’s just another pill. But it’s not. It’s a powerful, long-acting opioid with a narrow safety window for the heart. The data is clear. The guidelines are solid. What’s missing is consistent practice.
If you’re prescribing methadone: get an ECG before starting. Get it again after 3 weeks. Know the patient’s meds. Check their potassium. Ask about snoring. Track changes. Don’t assume they’re fine because they “feel okay.”
If you’re on methadone: ask for your QTc number. Ask how often you’ll be monitored. If they say “we don’t do that here,” push back. You deserve to know your heart is safe while you rebuild your life.
Can methadone cause sudden death even with normal QTc?
Yes, but it’s rare. Sudden death can still occur due to respiratory depression, overdose, or other factors like undiagnosed heart disease. However, when QTc is normal and no other risk factors are present, the risk of a lethal arrhythmia like Torsades de Pointes is very low. The biggest danger comes from QTc prolongation combined with other triggers - not methadone alone.
Is buprenorphine safer than methadone for the heart?
Yes. Buprenorphine has minimal effect on the hERG channel and causes little to no QT prolongation. Multiple studies show its cardiac safety profile is significantly better than methadone’s. For patients with risk factors like older age, female gender, or existing heart conditions, buprenorphine is often the preferred choice for opioid dependence treatment.
Do I need an ECG if I’m on less than 100 mg of methadone?
It depends. If you’re under 100 mg/day and have no other risk factors (no heart disease, no low potassium, no other QT-prolonging drugs), an ECG isn’t always required. But if you’re female, over 65, have sleep apnea, or take antidepressants - even a low dose can be risky. The guideline is: if any risk factors exist, get a baseline ECG.
Can I still take methadone if my QTc is 480 ms?
Yes - but you’re in the high-risk category. You’ll need monthly ECGs, electrolyte checks, and a review of all other medications. Your prescriber should consider reducing your dose by 10-20% and monitor closely. If QTc doesn’t improve or worsens, switching to buprenorphine should be seriously discussed.
Why isn’t everyone on methadone tested regularly?
Cost, access, and awareness. Many clinics lack ECG machines or trained staff. Some providers still believe QT prolongation is rare or not clinically significant. But evidence shows structured monitoring reduces cardiac events by two-thirds. The barrier isn’t medical - it’s systemic. Patients need to advocate for themselves, and clinics need to prioritize safety over convenience.
What’s clear: methadone is one of the most effective tools we have for opioid dependence. But like all powerful tools, it demands respect. Monitoring isn’t red tape. It’s the difference between a patient living a full life - and a preventable death.



John Cena
February 18, 2026 AT 13:02