Every time you pick up a prescription, you’re holding a document that could save your life-or hurt you if you don’t understand it. The label on your medicine bottle isn’t just a sticker with directions. It’s your safety net. And yet, most people grab it, toss it in their bag, and never look at it again until they’re confused-or worse, sick.
Here’s the hard truth: prescription label misunderstandings cause over 1.3 million medication errors in the U.S. every year. Nearly a quarter of those happen because someone misread the label. You don’t need to be a pharmacist to spot the red flags. You just need to ask the right questions.
What’s the real name of this medicine?
Pharmacies list both the brand name and the generic name on your label. But they don’t always make it easy to find. Sometimes the generic name is tucked in small print. Other times, it’s missing entirely. That’s a problem.
Let’s say your doctor prescribed Lyrica. You see that name on the bottle. But the pill looks nothing like the last one you took. That’s because Lyrica is the brand name. The generic is pregabalin. If you’re taking another medication that interacts with pregabalin, you need to know that’s what’s in your bottle.
Always ask: “Is this the generic version? What’s the generic name?” If the pharmacist says, “It’s the same thing,” ask them to spell it out. Write it down. Then check your other prescriptions. You might be taking two drugs with the same active ingredient-and doubling your dose without knowing it.
How exactly should I take this?
“Take one by mouth daily” sounds simple. But what does “daily” mean? Morning? Night? With food? On an empty stomach?
Some medications, like antibiotics, lose effectiveness if taken with dairy. Others, like thyroid pills, need to be taken on an empty stomach at least 30 minutes before eating. Blood pressure meds often work best in the morning. But if you’re on a diuretic, taking it at night means you’ll be up every two hours to pee.
Don’t assume. Ask: “Should I take this with food or without?” “Is there a specific time of day that works best?” “What happens if I miss a dose?”
And watch for abbreviations. “QD” means once daily. “BID” is twice daily. “QHS” means at bedtime. If you don’t know what they mean, say so. Most pharmacists will write it out in plain English if you ask.
What does this pill look like?
Ever opened a bottle and thought, “This doesn’t look right”? That’s not paranoia. It’s a red flag.
Medication errors happen when you get the wrong drug because the pill shape, color, or size changed. Maybe your insurance switched you to a different manufacturer. Maybe the pharmacy made a mistake. Either way, your job is to notice.
Ask: “Is this the same pill I got last time?” “What does it look like?” “Can you show me a picture or the actual bottle from the shelf?”
Pharmacists keep reference photos of pills. They’re trained to spot differences. If the color changed from blue to white, or the imprint changed from “A123” to “B456,” that’s worth asking about. Don’t be shy. A good pharmacist will appreciate you checking.
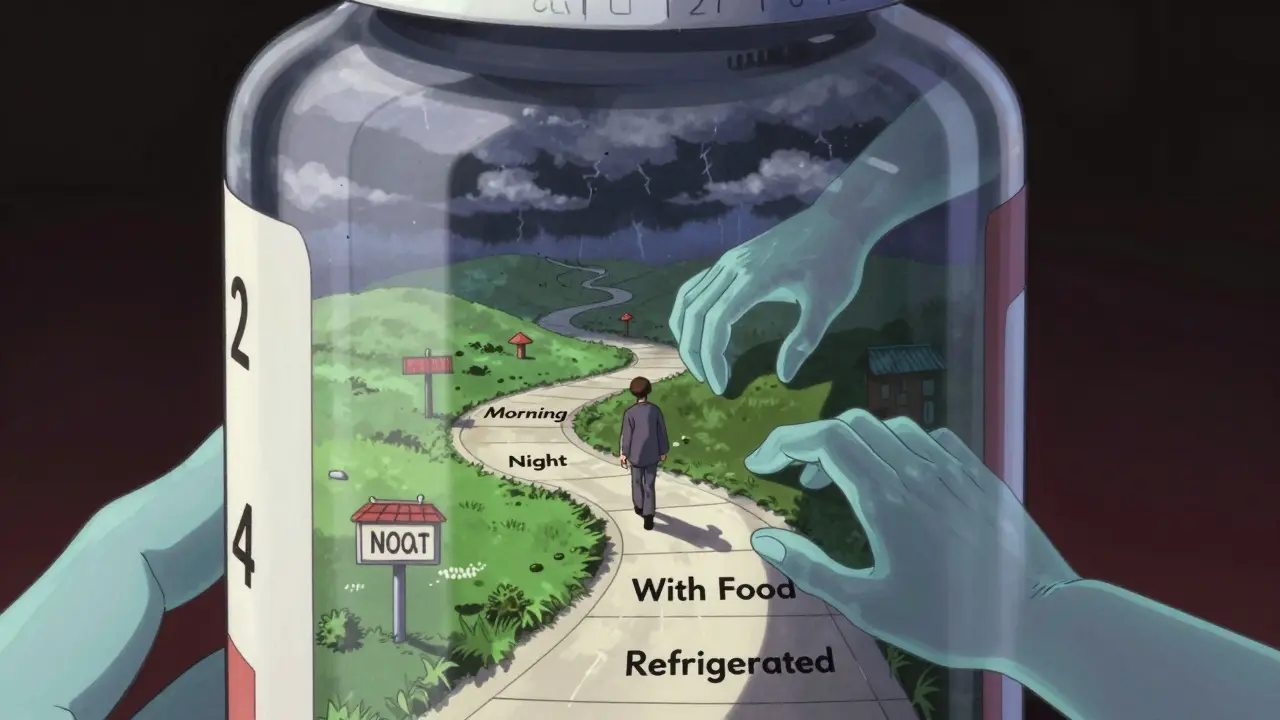
How long does this last?
Expiration dates aren’t just for show. The FDA requires them for a reason. After the date, the drug may lose strength-or, in rare cases, break down into something harmful.
But here’s what most people don’t know: some meds need special storage. Your insulin? Refrigerated. Your nitroglycerin? Keep it in its original glass bottle, away from light and heat. Your liquid antibiotics? Some need refrigeration even if the bottle doesn’t say so.
Ask: “Does this need to be kept in the fridge?” “Can I leave it in my car on a hot day?” “What happens if it gets too warm?”
One patient in a 2023 Consumer Reports survey kept her blood pressure medication at room temperature for two weeks because the storage instruction was printed in tiny font on the back of the label. She didn’t realize it needed to be cold. Her blood pressure spiked. She ended up in the ER.
How many refills do I have left?
This one seems obvious. But people forget. They run out. They call the doctor. The doctor calls the pharmacy. The pharmacy says, “No refills left.” And now you’re stuck.
Ask: “How many refills are on this prescription?” “When will I need to get a new one?” “Can you send a refill request to my doctor automatically?”
Some pharmacies offer auto-refill programs. Others don’t. If you’re on a chronic medication-like high blood pressure, diabetes, or thyroid pills-ask if you can set up automatic refills. It saves time, and it prevents dangerous gaps in treatment.
What are the side effects I should watch for?
Side effects are listed on the Medication Guide, but that’s a separate sheet. Most people don’t read it. And if they do, they get scared by a list of 20 possible reactions.
Ask: “What are the top three side effects I should know about?” “Which ones mean I need to call you right away?” “Is there anything I should avoid while taking this?”
For example, if you’re on an opioid, you need to know that drowsiness plus alcohol can stop your breathing. If you’re on statins, muscle pain could be a sign of a serious reaction. If you’re on an antidepressant, suicidal thoughts in the first few weeks are rare-but real.
Don’t just accept “some people get headaches.” Ask for the ones that matter. The ones that are dangerous.
Can this interact with other meds or foods?
You’re not just taking one drug. You’re probably taking several. Your blood pressure pill. Your vitamin D. Your ibuprofen for the knee pain. Your grapefruit juice in the morning.
Some combinations are deadly. Statins with grapefruit juice can cause muscle damage. Blood thinners with NSAIDs like ibuprofen raise your risk of bleeding. Antibiotics with dairy reduce absorption.
Ask: “Does this interact with anything else I’m taking?” “What about my vitamins or supplements?” “Can I drink alcohol with this?”
Bring a list of everything you take-even the herbal teas and over-the-counter pills. Pharmacists can check for interactions in seconds. Don’t make them guess.
Is there a simpler way to take this?
Some prescriptions come in pills you have to split. Others are liquids you have to measure. Some require multiple doses a day. That’s a recipe for mistakes.
Ask: “Is there a once-daily version?” “Can this be switched to a patch or injection?” “Do you have a pill splitter or a dosing cup?”
For older adults or people with arthritis, a once-daily pill is safer than three pills a day. For someone with vision problems, a liquid with a dosing syringe is better than tiny tablets.
Pharmacies have tools. They have blister packs. They have pre-filled pill organizers. Ask if they can help you simplify your regimen. It’s not just convenience-it’s safety.
Can I get this in large print or another language?
One in three U.S. adults has trouble reading health materials. That’s not about intelligence. It’s about health literacy.
Ask: “Can you print this label in larger font?” “Do you have a version in Spanish, Tagalog, or another language?” “Can you explain it to me out loud?”
By law, pharmacies that take Medicare or Medicaid must offer translation services. Many independent pharmacies already do it. You don’t need to be fluent in English to get safe care. You just need to ask.
Large-print labels are available at 92% of U.S. pharmacies. But you have to request them. No one will offer unless you say something.
What if I still don’t understand?
It’s okay to say, “I’m still confused.”
Ask: “Can I call you later if I have more questions?” “Do you have a nurse or pharmacist I can talk to?” “Is there a video or website that explains this?”
More than half of U.S. pharmacies now offer QR codes on labels that link to short video instructions. Scan it with your phone. Watch it. Pause it. Rewind it. That’s not magic. That’s modern care.
And if you’re still unsure? Call the pharmacy back. Or ask your doctor for clarification. Medication safety isn’t a one-time check at the counter. It’s an ongoing conversation.
Spending two minutes asking these questions can prevent hospital visits, ER trips, and even death. You’re not being difficult. You’re being smart.
The system isn’t perfect. Labels are cluttered. Font sizes vary. Instructions are inconsistent. But you’re not powerless. You hold the final check. You’re the last line of defense. And that’s worth speaking up for.


Cassie Widders
January 12, 2026 AT 19:05I always just glance at the label and hope for the best. But after reading this, I’m going to actually read it next time. Seriously, two minutes could save your life.
Thanks for laying it out so simply.
Amanda Eichstaedt
January 12, 2026 AT 20:54This is the kind of stuff no one teaches you but everyone needs to know. I used to take my blood pressure med with grapefruit juice because ‘it tastes better.’ Turns out that’s a dumb way to end up in the ER.
Now I ask every single question on this list. Pharmacists think I’m weird. I think they’re underpaid heroes.
Jose Mecanico
January 14, 2026 AT 14:36Good list. I’ve seen people get the wrong meds because they didn’t check the pill shape. One guy took his neighbor’s anxiety med by accident-same size, same color. He ended up in a psych ward.
Always double-check. It’s not paranoia. It’s responsibility.
Alex Fortwengler
January 15, 2026 AT 20:05Of course the label’s confusing. Big Pharma and the FDA want you confused. Why? So you keep buying their overpriced crap and don’t realize the generic is just as good. They don’t want you asking questions-they want you compliant.
And don’t get me started on QR codes. That’s surveillance disguised as ‘convenience.’
Read the damn label. But don’t trust the system. Trust yourself.
jordan shiyangeni
January 16, 2026 AT 04:34It’s astonishing how many people treat pharmaceuticals like they’re buying a bag of chips from a vending machine. The fact that 1.3 million medication errors occur annually isn’t a failure of labeling-it’s a failure of civic literacy. People refuse to engage with basic health information because they’ve been conditioned to outsource all responsibility to ‘experts.’
And yet, when someone actually takes initiative-like asking about drug interactions or storage conditions-they’re labeled ‘difficult.’ No. You’re the only adult in the room. The pharmacist is overworked. Your doctor is rushed. You are the final checkpoint. And if you don’t act, who will? The system won’t save you. You have to save yourself. Period.
Abner San Diego
January 16, 2026 AT 06:02Why are we even talking about this? In America, if you can’t read a pill bottle, maybe you shouldn’t be on meds. Get your act together. This isn’t rocket science. It’s basic reading. If you need a translator or large print, fine-but don’t make the whole system bend for people who refuse to try.
Also, grapefruit juice? That’s not a ‘risk,’ that’s just dumb. Stop blaming the label and start using your brain.
Eileen Reilly
January 17, 2026 AT 21:37OMG I JUST REALIZED I’VE BEEN TAKING MY ANTIBIOTIC WITH MILK FOR 3 WEEKS 😭😭😭
thx for the wake up call. also why do they put the generic name in 4pt font like it’s a secret? #pharmacyconspiracy
Monica Puglia
January 18, 2026 AT 03:28Thank you for this. 🙏 I work with elderly patients and so many of them don’t ask because they’re embarrassed or afraid they’ll sound stupid. But you’re right-it’s not about being smart. It’s about being safe.
My grandma started using the large-print labels after this and she hasn’t missed a dose since. Also, she loves the QR code videos. 📱❤️
Keep spreading this info. It matters.