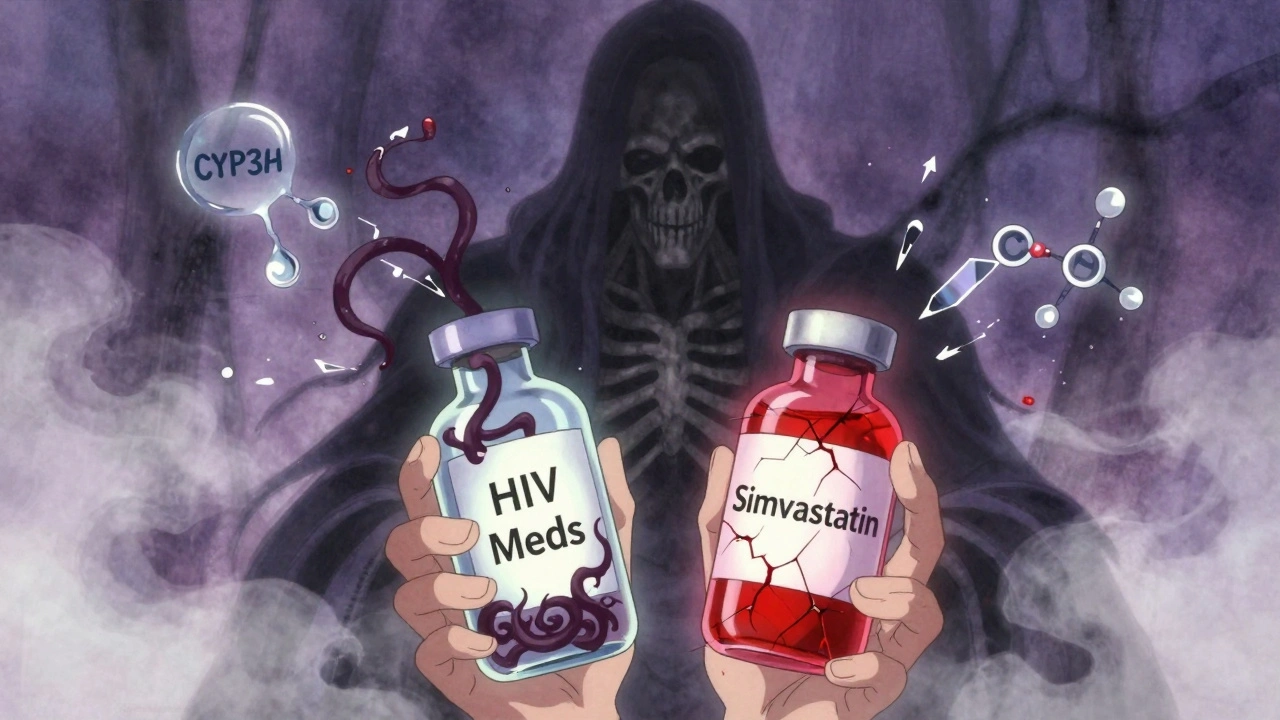
Atorvastatin with Cobicistat: Drug Interactions and Safety Risks
When you take atorvastatin with cobicistat, a combination of a cholesterol-lowering statin and a drug that blocks liver enzymes to boost other medications. Also known as atorvastatin and cobicistat interaction, this mix can push atorvastatin levels in your blood to unsafe heights—raising the risk of muscle damage, kidney stress, and liver issues. Cobicistat doesn’t just help HIV meds work better; it shuts down the CYP3A4 enzyme, which your body normally uses to break down atorvastatin. That means your body can’t clear the statin fast enough, and it builds up like a clogged drain.
This isn’t theoretical. Studies show people on this combo have up to a 4-fold increase in atorvastatin exposure. That’s why the FDA and drug manufacturers warn against using high doses of atorvastatin (over 20 mg daily) with cobicistat. Even 10 mg can be risky if you’re older, have kidney trouble, or take other meds that affect the same pathway. You might not feel anything at first—but muscle pain, dark urine, or unexplained fatigue could be early signs of rhabdomyolysis, a serious condition where muscle tissue breaks down and floods your kidneys.
It’s not just about atorvastatin. Cobicistat messes with dozens of drugs, including other statins like simvastatin and lovastatin, which are even more sensitive. That’s why doctors often switch you to pravastatin or rosuvastatin—drugs that don’t rely as much on CYP3A4. If you’re on HIV treatment with cobicistat and also need cholesterol control, your pharmacist should be checking your full list of pills, not just the big ones. Even over-the-counter supplements like St. John’s wort or grapefruit juice can make this worse, since they also interfere with liver enzymes.
Many people don’t realize their HIV meds are the hidden culprit behind new muscle pain or liver test abnormalities. If you’ve started cobicistat recently and noticed new side effects, it’s not just bad luck—it’s a known interaction. Your doctor doesn’t always know every combo risk, especially when prescriptions come from different specialists. That’s why checking for interactions isn’t just a good habit—it’s a safety must.
Below, you’ll find real-world advice from people who’ve been there: how to spot warning signs early, what safer alternatives exist, how pharmacists navigate these combos, and why even small changes in your meds can have big consequences. This isn’t about fear—it’s about knowing what to ask for, what to watch for, and how to keep your treatment working without putting your body at risk.