When you have a sore knee or aching shoulder, you might reach for a pill-or a cream. But here’s the thing: topical and oral meds don’t work the same way inside your body. One goes straight to the pain. The other floods your whole system. And that difference changes everything-especially when it comes to safety.
How Your Body Handles Topical vs. Oral Meds
Topical medications-gels, creams, patches-go on your skin. They’re meant to stay local. Think of them like a targeted spray: you hit the sore spot, and the drug works right there. Less than 5% of the dose usually makes it into your bloodstream. That’s why doctors now recommend topical NSAIDs like diclofenac gel as the first choice for joint pain, especially in older adults. The American College of Rheumatology says it outright: start with the cream, not the pill. Oral meds, on the other hand, are built to travel. You swallow a pill, it dissolves in your stomach, gets absorbed through your gut, then heads straight to your liver. That’s where things get tricky. Your liver doesn’t just let everything pass through. It breaks down a chunk of the drug before it even reaches your bloodstream. This is called first-pass metabolism. For some drugs, like morphine, up to 95% of the dose gets destroyed before it can do its job. Even common painkillers like ibuprofen lose 30-50% of their strength on the way in. What’s left? A full-body dose.Why Systemic Absorption Matters for Safety
The more drug that gets into your blood, the more places it can cause trouble. Oral NSAIDs are linked to stomach ulcers, kidney damage, and heart risks. In clinical trials, about 15% of people taking oral NSAIDs regularly develop gastrointestinal problems. That’s 1 in 7. For topical NSAIDs? Less than 1%. The numbers don’t lie: the FDA’s adverse event database shows 14.7 serious incidents per 10,000 oral NSAID prescriptions versus just 1.2 per 10,000 for topical ones. But here’s a myth that needs busting: topical doesn’t mean zero absorption. If you apply a large amount-say, a full tube of gel over your back and shoulders-or if your skin is damaged, cracked, or thin (common in older adults), more drug can seep in. There are documented cases where topical diclofenac reached plasma levels high enough to cause liver stress or high blood pressure. The European League Against Rheumatism found that absorption rates can vary by 300-400% between people using the same dose. One person gets relief with a dime-sized dab. Another needs a full strip. It’s not just about the product-it’s about your skin, your age, your health.Real-World Outcomes: Pain Relief and Patient Experience
Do topical meds actually work? Yes. In a 2023 survey of over 2,400 people with osteoarthritis, 68% reported good to excellent pain relief with topical NSAIDs. That’s only 4% lower than oral pills. But here’s what changed their minds: 89% preferred the cream because they didn’t get stomach upset. On Reddit’s chronic pain forums, people regularly say things like, “No more acid reflux since switching to gel,” or “I finally slept through the night without popping pills.” But it’s not perfect. Some users complain about messiness, slow absorption in cold weather, or not feeling enough relief for severe pain. And that’s the trade-off. Topical meds are great for localized pain-knees, elbows, lower back. They’re not going to help with a full-body flu or an infected tooth. Only about 12% of the 200 most common prescription drugs can even be made into topical form. Why? Because most molecules are too big to slip through your skin.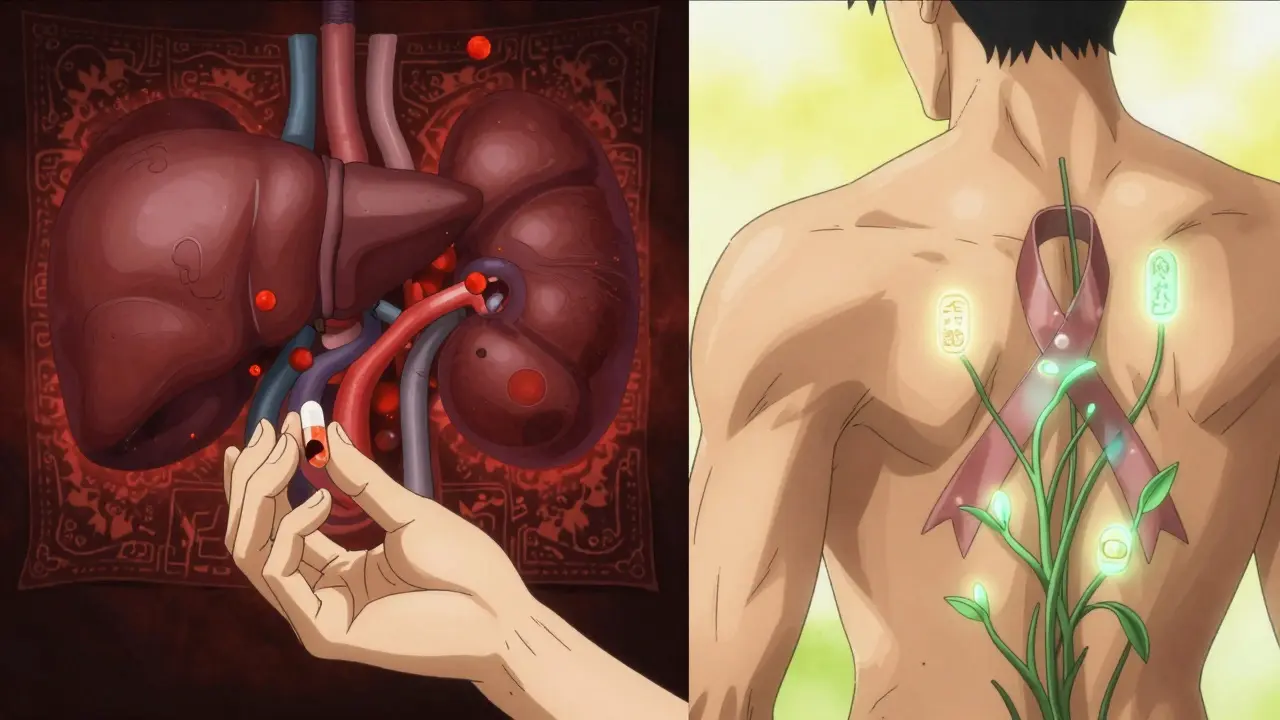
Who Benefits Most From Topical Meds?
The answer is simple: older adults and people with chronic conditions. The American Geriatrics Society’s Beers Criteria-used by doctors nationwide to avoid risky prescriptions-explicitly says: avoid oral NSAIDs in seniors. Use topical instead. Why? Because older people are more likely to have stomach issues, kidney problems, or take multiple medications that interact badly with pills. Topical delivery cuts the risk of GI bleeding by 82% compared to oral NSAIDs. It also helps with adherence. A 2023 study tracked 1,842 Medicare patients over a year. Those on topical meds were 37% more likely to stick with their treatment than those on pills. Why? No swallowing trouble. No pill boxes to organize. No fear of side effects. For someone with arthritis who’s already juggling five other meds, that’s huge.What You Need to Know to Use Topical Meds Right
Applying a topical cream isn’t as simple as smearing it on. The American Academy of Dermatology says you need a 4-6 inch ribbon of gel, applied 3-4 times a day. Too little? You won’t get relief. Too much? You risk systemic absorption. And temperature matters. Skin absorbs better when it’s warm. If it’s winter and your hands are cold, the gel won’t soak in as well. Rubbing it in helps-but don’t overdo it. Don’t cover the area with plastic wrap unless your doctor says to. And never apply it to broken skin unless instructed. Also, check the label. Only 43% of over-the-counter topical products give clear instructions on how much to use or how to maximize absorption. Most people wing it. That’s why pharmacists report that 41% of topical treatment failures come from wrong application-not because the drug doesn’t work.
The Bigger Picture: Why This Shift Is Happening
The market is changing fast. The global topical drug market hit $52.3 billion in 2023 and is growing at 7.2% a year-nearly twice as fast as oral meds. Why? Because hospitals are seeing fewer NSAID-related emergencies. In 2023, 18,432 hospitalizations in the U.S. were tied to oral NSAID stomach damage. Only 127 came from topical NSAIDs. Insurance companies noticed. Medicare Part D now covers 82% of topical NSAID prescriptions versus just 67% for oral ones. Even the FDA is making it easier to approve new topical formulations if they prove they stay mostly local. Big pharma is investing too. Johnson & Johnson spent $487 million on topical research in 2023. Novartis moved 15% of its oral NSAID budget to transdermal projects. Why? Because the future isn’t just about making pills. It’s about making them safer.The Future: Microneedles and Beyond
New tech is blurring the line. Microneedle patches-tiny needles that dissolve into the skin-are in late-stage trials. They’re designed to deliver drugs that used to require pills, like osteoporosis meds. Early results show 45% bioavailability-way higher than traditional topical, but still lower than oral. That’s the sweet spot: enough to work, not enough to harm. But there’s a wall. Most drugs over 500 Daltons (a unit of molecular weight) can’t cross the skin barrier. That’s why antibiotics, antidepressants, and many heart meds still come as pills. Science is working on it-penetration enhancers, lipid carriers, nanotechnology-but it’s slow.Bottom Line: Choose Based on Your Body, Not Just Convenience
If your pain is in one spot-knee, shoulder, elbow-start with the cream. It’s safer, just as effective for most people, and you’re far less likely to end up in the ER. If your pain is everywhere, or you’re treating an infection or systemic condition, pills are still necessary. But don’t assume oral is the default. Ask your doctor: “Is there a topical version?” The data is clear: for localized pain, topical meds are the smarter choice. Not because they’re trendy. But because they work better for your body-and leave your stomach, kidneys, and heart alone.Are topical medications completely safe?
No medication is completely risk-free. Topical meds are much safer than oral ones for most people, but they can still cause skin irritation, allergic reactions, or, in rare cases, systemic effects if applied too generously or on damaged skin. Always follow the dosage instructions and avoid using large amounts over large areas without medical advice.
Can I use topical NSAIDs if I have a stomach ulcer?
Yes, topical NSAIDs are generally safe for people with stomach ulcers because they don’t significantly enter your bloodstream. Unlike oral NSAIDs, which irritate the stomach lining directly, topical versions target pain locally. However, always check with your doctor before switching, especially if you’re on blood thinners or have kidney issues.
Why doesn’t my topical cream seem to work?
You might be using too little, too infrequently, or on cold skin. Most people underapply topical meds. Use a 4-6 inch ribbon (about the size of a golf ball) and apply it 3-4 times a day. Rub it in gently and wait 10 minutes before covering with clothing. Warm skin absorbs better-so if it’s winter, warm the area with a towel first.
Is it okay to use both topical and oral NSAIDs together?
Generally, no. Combining them increases your total NSAID exposure and raises the risk of side effects-even if one is topical. Your body still absorbs some of the cream, and adding a pill can push you over the safety limit. Only do this under direct supervision from a doctor who’s monitoring your kidney and liver function.
Do topical meds work faster than pills?
It depends. Oral NSAIDs usually hit peak levels in 1-2 hours. Topical versions take longer-often 2-4 hours for noticeable relief. But they last longer without the spikes and crashes you get with pills. Many users report more consistent comfort over the day, even if the initial relief feels slower.
Can I use topical meds for back pain?
Yes, especially for lower back pain caused by muscle strain or arthritis. But you need to cover a large enough area-about the size of your palm or larger. If the pain is deep in the spine or radiating down your leg, topical meds alone won’t be enough. They work best for surface-level or muscle-based pain, not nerve or disc issues.
Are there topical antibiotics?
Yes, but only for skin infections like impetigo or minor cuts. Topical antibiotics like mupirocin or neomycin can’t treat internal infections like pneumonia or UTIs. They’re too strong to use systemically and won’t reach deep tissues. For those, you still need oral or IV antibiotics.
Why are topical meds more expensive than pills?
They often are-but not always. Generic oral NSAIDs cost less than $5 per month. Some topical gels run $30-$50. But insurance coverage is improving. Medicare now covers 82% of topical NSAID prescriptions, and many plans have lower copays for them because they reduce hospital visits. When you factor in fewer side effects, doctor visits, and GI treatments, topical meds can be cheaper overall.



Natasha Sandra
December 26, 2025 AT 09:39OMG I switched to diclofenac gel last winter and my knees haven’t felt this good in YEARS 😭 No more stomach burning at 3am! Also, my dog now licks my leg when I apply it-she thinks it’s ice cream. 🍦✨
Sophia Daniels
December 26, 2025 AT 20:55Let’s be real-America’s obsession with pills is why we’re the sick nation. Topical meds? That’s common sense. The FDA’s finally catching up. Meanwhile, Big Pharma’s still peddling poison in capsules like it’s 1999. 🇺🇸🔥 If you’re still popping ibuprofen like candy, you’re not just dumb-you’re a walking liability.
Steven Destiny
December 28, 2025 AT 02:49Stop overthinking this. If you’ve got a sore knee, use the gel. If you’ve got full-body pain, take the pill. Simple. No drama. I’ve been using both for 12 years-topical for knees, oral for migraines. Works. Done. Stop arguing and start healing.
Fabio Raphael
December 28, 2025 AT 04:35I’ve been reading this whole post and I just want to say-thank you. This is the kind of clear, science-backed info that’s so rare online. I’m 71 and on 7 meds already. The idea that I could reduce my GI risks just by switching to a cream? That’s life-changing. I’m showing this to my doctor tomorrow.
Amy Lesleighter (Wales)
December 29, 2025 AT 19:14topical = less junk in your blood. pills = your liver does the work. if your liver is tired from meds, alcohol, or just life… why make it worse? i started using the gel for my back and now i sleep like a baby. no more 3am panic about stomach pain. simple stuff. why do we make it hard?
Becky Baker
December 29, 2025 AT 20:49Topical meds are for weak people who can’t handle a real pill. If you can’t swallow a tablet, maybe you shouldn’t be managing your own pain. I’ve been on NSAIDs since I was 25 and I’m still running marathons. Stop coddling yourself.
Rajni Jain
December 29, 2025 AT 21:08i live in india and we use a lot of herbal pastes for pain… but this article made me realize… maybe we dont need to overcomplicate it. my aunt used to rub coconut oil + turmeric on her knees and she’s 82 and walks 5km daily. sometimes the simplest things work best. thank you for this
Erwin Asilom
December 29, 2025 AT 22:04One point often missed: topical NSAIDs require consistent application. Most users apply once or twice daily. The studies show 3-4 applications are needed for optimal effect. If you’re not seeing results, it’s not the drug-it’s the routine. Also, warm skin = better absorption. A quick warm towel before application makes a measurable difference.
Sumler Luu
December 31, 2025 AT 12:11Just wanted to add-don’t forget the placebo effect. I tried the gel after months of pills and felt better immediately… but then I realized I’d applied it right before a hot shower. Was it the gel or the warmth? Who knows. But I’m still using it. If it helps, even a little, it’s worth it.