Clinician Drug Prices: What You Need to Know About Cost, Access, and Fairness
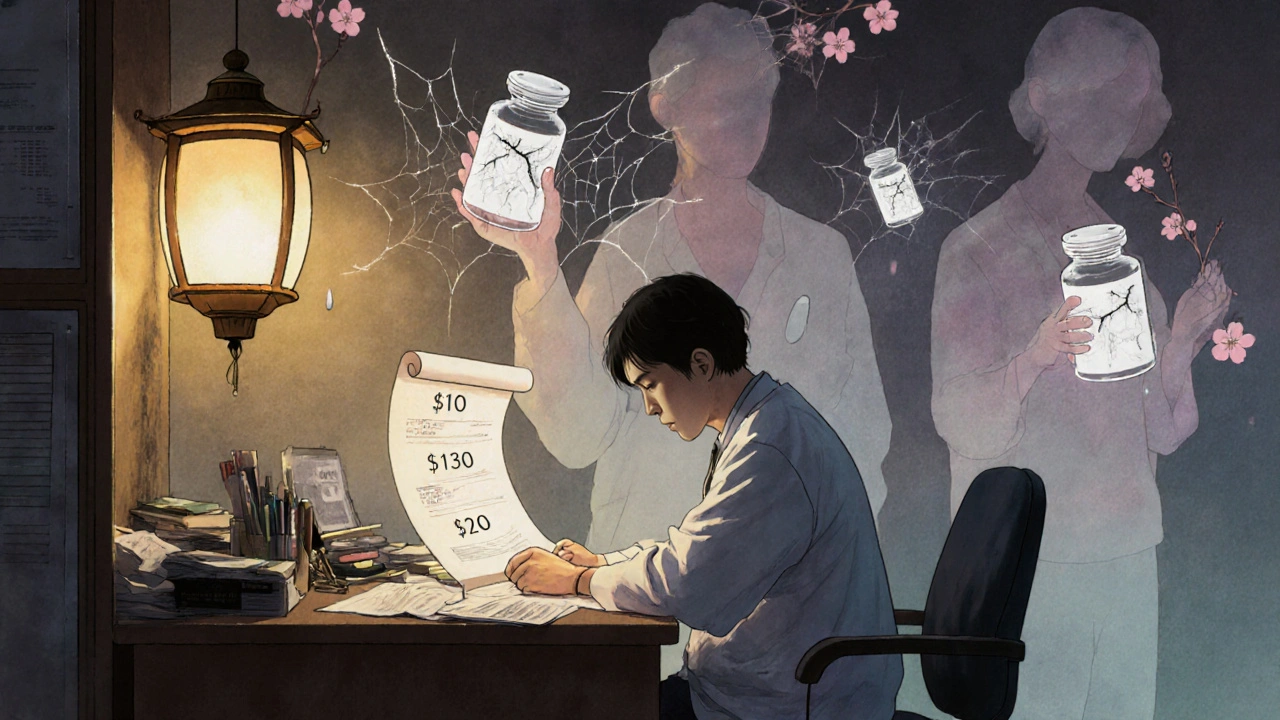
When doctors prescribe a medication, they don’t always know how much it will cost the patient—that’s the harsh reality of clinician drug prices, the out-of-pocket costs patients face when filling prescriptions, often with little warning or transparency. Also known as patient drug costs, these prices are shaped by everything from manufacturing rules to insurance policies, and they directly impact whether someone takes their medicine or skips it altogether.
Behind every prescription is a system that doesn’t always add up. The same generic version of metformin might cost $4 at one pharmacy and $45 at another, even just a few miles apart. Why? Because generic drug pricing, the cost of non-brand-name medications that are chemically identical to their branded counterparts. Also known as off-patent drug costs, these prices vary based on supply chains, regional distribution deals, and pharmacy benefit managers. It’s not about quality—it’s about who’s paying, and how. And for many patients, especially those on fixed incomes or without good insurance, that difference means skipping doses, splitting pills, or going without.
These price gaps aren’t random. They’re tied to how drugs are made, who controls distribution, and whether a country allows direct price negotiations. In places like Canada, government oversight keeps many drug prices lower. In the U.S., pharmacy chains and insurers often set prices without public input. Meanwhile, medication affordability, the ability of patients to pay for necessary drugs without financial hardship. Also known as drug access equity, this is a growing crisis—one that shows up in emergency rooms, in skipped insulin doses, and in patients choosing between rent and refills.
What does this mean for clinicians? They’re caught in the middle. They know what a patient needs, but they can’t control the price tag. That’s why so many posts on this site focus on alternatives, generics, and how to find the lowest cost without sacrificing safety. You’ll find guides on how to check drug prices before filling a script, how to use patient assistance programs, and why the same pill can cost different amounts depending on where you live.
Some of the most urgent stories here aren’t about new drugs—they’re about old ones that suddenly become unaffordable. You’ll read about how counterfeit pills sneak into the market with deadly contaminants, how bioavailability studies ensure generics work the same, and how alcohol and diabetes meds can turn a simple prescription into a life-threatening mix. These aren’t edge cases. They’re everyday realities for millions.
Whether you’re a patient trying to stretch your budget, a caregiver worried about a loved one’s meds, or a clinician looking for better ways to help, this collection gives you the real facts—not the marketing. No fluff. No jargon. Just what you need to know to make smarter choices about drug costs, access, and safety.