People say they feel "dizzy" all the time. But if you’ve ever had vertigo, you know it’s not the same thing. One feels like the room is spinning. The other feels like you’re about to pass out. They’re not interchangeable. And mistaking one for the other can delay real treatment-sometimes for years.
Vertigo Isn’t Just Dizziness
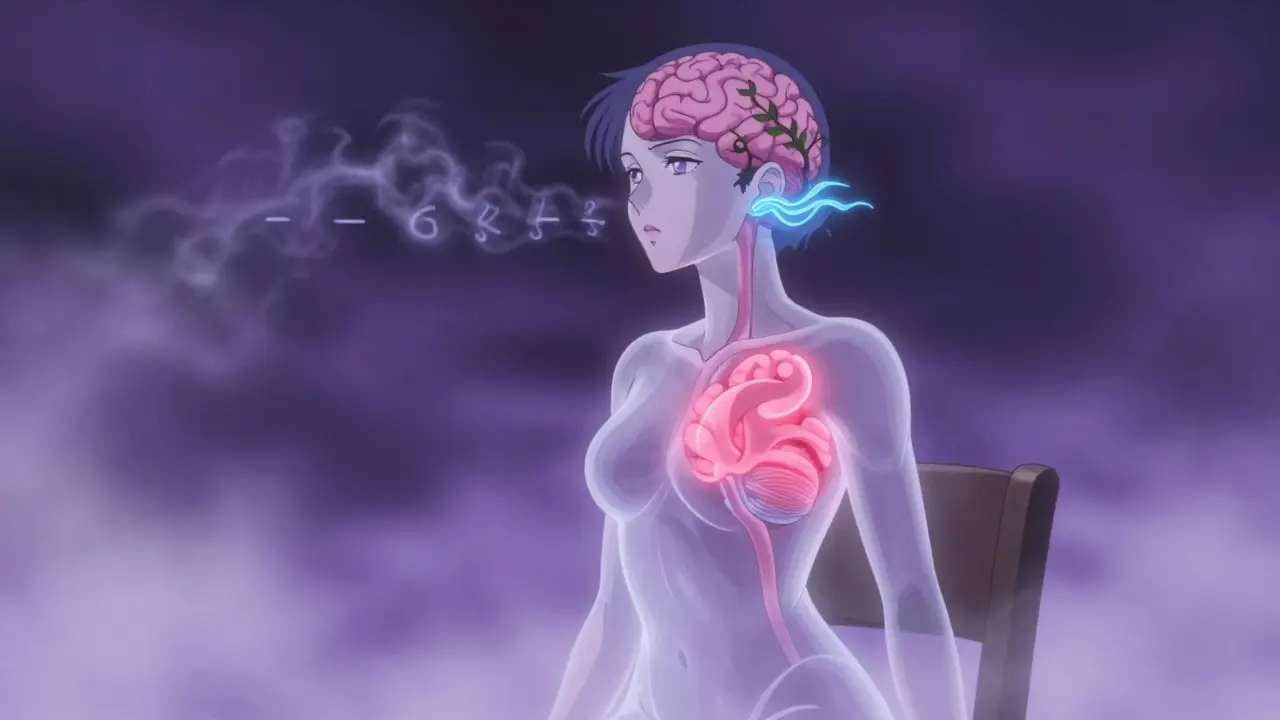
Vertigo isn’t a vague feeling of unsteadiness. It’s a specific illusion: you or the world around you is moving, usually spinning. You’re sitting still, but your brain says you’re on a merry-go-round. That’s not anxiety. That’s your vestibular system sending false signals. It’s like your inner ear is screaming, "We’re turning!"-even when you’re not.
Dizziness? That’s different. It’s lightheadedness. A foggy head. A sense you might faint. You don’t feel rotation. You just feel off. It’s what happens when your blood pressure drops too fast standing up, when you’re low on iron, or when meds mess with your balance. It’s not a spinning sensation. It’s a sinking one.
That distinction matters because the causes are worlds apart. And so are the treatments.
Why Your Inner Ear Is the Key
Your inner ear isn’t just for hearing. It’s your body’s gyroscope. Three fluid-filled semicircular canals detect head rotation. Tiny crystals (otoconia) in the utricle and saccule sense gravity and straight-line movement. Together, they send data to your brain 100 to 200 milliseconds after you move. That’s faster than you can blink.
When those crystals get loose-like in Benign Paroxysmal Positional Vertigo (BPPV)-they float into the wrong canal. Every time you roll over or look up, they jiggle the fluid, tricking your brain into thinking you’re spinning. BPPV is the #1 cause of vertigo. It affects 2.4% of people every year. Half of those are over 50.
That’s why the Epley maneuver works. It’s not magic. It’s physics. A series of controlled head movements, done right, guides those loose crystals back where they belong. Success rate? 80-90%. Most people feel better after one or two sessions. Yet, many go months-or years-misdiagnosed as having "anxiety" or "aging."
Neurological Vertigo: When the Brain Lies
Not all vertigo comes from the ear. Sometimes, it comes from the brain.
When a stroke hits the brainstem or cerebellum, it can disrupt how vestibular signals are processed. That’s central vertigo. It’s rare-only 5-10% of cases-but dangerous. Unlike BPPV, it doesn’t just happen when you turn your head. It’s constant. And it often comes with other red flags: double vision, slurred speech, numbness on one side, or trouble walking in a straight line.
Multiple sclerosis can do the same. So can vestibular migraine. That’s right-migraines don’t always mean headaches. Some people get vertigo as their only symptom. They feel like they’re on a boat, nauseated, sensitive to light, and then it fades. Doctors often mistake this for inner ear infections. But if you’ve had migraines before, or if your vertigo episodes last hours and come with nausea, it’s likely vestibular migraine. It makes up 7-10% of all vertigo cases.
Here’s the catch: central vertigo doesn’t usually cause hearing loss. Peripheral vertigo (from the ear) often does. If you suddenly lose hearing on one side with vertigo, that’s not BPPV. That’s something more serious.
Dizziness: The Broad Category With Many Faces
Dizziness isn’t one condition. It’s a symptom with dozens of causes.
Cardiovascular issues are the biggest culprit-about 20-30% of cases. Orthostatic hypotension: your blood pressure drops too much when you stand. You feel faint. Your vision tunnels. You might even black out. It’s common in older adults, especially if they’re on blood pressure meds.
Anemia and low blood sugar? They’re next. When your brain doesn’t get enough oxygen or glucose, it doesn’t function right. You feel dizzy, tired, confused. Easy to fix-once you know the cause.
Then there’s medication. Antibiotics like gentamicin can damage your inner ear. Blood pressure pills, antidepressants, even some allergy meds can throw off your balance. If your dizziness started after a new prescription, talk to your doctor. Don’t assume it’s just "getting older."
And then there’s psychological dizziness. Anxiety doesn’t cause vertigo, but it can make you hypersensitive to normal balance signals. That’s Persistent Postural-Perceptual Dizziness (PPPD). It often follows a real vestibular event-like an infection or BPPV-that never fully resolved. Your brain gets stuck in "alarm mode." You feel off even when you’re calm. It’s real. It’s not "all in your head." It’s your nervous system overreacting.
How Doctors Tell the Difference
There’s no single blood test for vertigo or dizziness. Diagnosis is all about clues.
Doctors start with history: When did it start? What triggers it? How long does it last? Do you hear ringing? Lose hearing? Have headaches? Numbness?
Then comes the physical exam. The head impulse test checks if your inner ear reflexes work. If your eyes jerk when you quickly turn your head, it points to vestibular neuritis. If your eyes move involuntarily in a rhythmic pattern (nystagmus), the direction and timing tell you if it’s peripheral or central.
Videonystagmography (VNG) is the gold standard. You wear special goggles while your eyes are tracked as you follow lights and get cold/warm air blown into your ears. It shows exactly how well your vestibular system is firing. It’s 95% accurate for peripheral problems.
But here’s the problem: only 12% of primary care doctors feel confident diagnosing vertigo. Most rely on guesswork. That’s why delays are so common. People wait 8 months on average before getting the right diagnosis. BPPV patients get answers faster-around 3 months. Those with Ménière’s disease? Nearly 15 months.
What Actually Helps
Treatment depends entirely on the cause.
For BPPV: Epley maneuver. Done in a clinic or at home with guidance. Takes 10-15 minutes. Works in most cases.
For vestibular neuritis: Short-term steroids to reduce inflammation, then vestibular rehabilitation. That’s physical therapy for your balance system. Exercises to retrain your brain to trust signals from your inner ear again. It takes 6-8 weeks. But 89% of people who stick with it see major improvement.
For vestibular migraine: Avoid triggers-stress, caffeine, skipped meals. Some people take daily migraine preventatives like beta-blockers or topiramate. New FDA-approved protocols for transtympanic gentamicin can help severe, frequent attacks.
For cardiovascular dizziness: Adjust meds, increase salt and water intake, rise slowly. For anemia: iron supplements. For PPPD: cognitive behavioral therapy (CBT) combined with balance retraining. It’s not about fixing your inner ear-it’s about calming your nervous system.
And for stroke-related vertigo? That’s an emergency. If you have vertigo with new weakness, slurred speech, or double vision-call 911. Don’t wait. Don’t assume it’s just a bad ear infection.

What Doesn’t Work
Antibiotics for "ear infection" when there’s no infection. Anti-nausea meds alone for BPPV. SSRIs for dizziness without anxiety. And the worst: telling someone their vertigo is "just stress."
Over 30% of vestibular migraine cases are misdiagnosed as sinusitis or anxiety. One patient spent two years on antidepressants before a specialist found the real cause: migraines triggered by sleep loss and screen glare.
And here’s the hard truth: if you have PPPD and no one tells you what it is, you’ll keep cycling through doctors, tests, and meds that don’t touch the root problem. You’ll feel dismissed. You’re not crazy. Your brain just got stuck in a loop.
The Bigger Picture
The global market for vertigo treatments is growing fast-$2.8 billion in 2022 and climbing. Why? Because more people are being diagnosed. More hospitals are offering vestibular rehab. Medicare now pays $235 per VNG test-up from $185 in 2020.
But access is uneven. Only 42% of community hospitals have specialized vestibular programs. Academic centers? 78%. That means if you live outside a big city, you might need to travel for the right care.
And the population is aging. One in three adults over 65 has dizziness. By 2030, demand for vestibular services will jump 25%. We’re not ready.
Research is moving fast too. Stanford is testing hair cell regeneration. Johns Hopkins has AI that can read eye movements and tell if vertigo is from the ear or the brain-with 85% accuracy. That could change ER diagnostics overnight.
What You Can Do Now
If you’re dizzy or spinning:
- Write down your symptoms: When? How long? What triggers it? Any hearing loss? Headache? Numbness?
- Don’t assume it’s stress. Don’t self-diagnose with Google.
- Ask your doctor for a head impulse test or VNG. If they don’t know what that is, ask for a referral to an ENT or neurotologist.
- If you have vertigo with new neurological symptoms-go to the ER.
- If you have BPPV, ask for the Epley maneuver. Don’t wait.
- If you’ve had dizziness for months with no diagnosis, seek out a vestibular therapist. They’re certified. They know what they’re doing.
You don’t have to live with this. The right diagnosis isn’t magic. It’s science. And it’s available-if you know what to ask for.



Ian Cheung
January 10, 2026 AT 09:58Vertigo hit me like a freight train while brushing my teeth one morning
I thought I was dying or having a stroke
Turned out it was loose crystals in my ear
One Epley maneuver later and I was fine
Doctors kept calling it anxiety
Turns out my inner ear was just being a drama queen
Dwayne Dickson
January 12, 2026 AT 04:47The clinical distinction between peripheral and central vertigo remains critically underappreciated in primary care settings, despite its profound implications for diagnostic triage and therapeutic intervention.
The vestibular system’s neuroanatomical architecture-particularly the semicircular canals and otolith organs-functions as a high-fidelity inertial navigation system, and its dysregulation precipitates distinct phenomenological profiles.
Benign paroxysmal positional vertigo (BPPV), characterized by transient, positionally triggered nystagmus, is not merely a benign nuisance but a quantifiable biomechanical displacement of otoconial debris.
Conversely, central vertigo arising from brainstem or cerebellar pathology manifests as non-position-dependent, persistent dizziness, often accompanied by neurological red flags such as dysarthria, diplopia, or ataxia.
It is both alarming and regrettably common for patients to undergo prolonged, ineffective pharmacological regimens for presumed anxiety or migraine when the root etiology is mechanically remediable.
The Epley maneuver, a simple, non-invasive, physics-based repositioning technique, achieves success rates exceeding 85% in properly diagnosed cases.
Yet, the absence of standardized vestibular screening protocols in general practice perpetuates diagnostic delay, with median time-to-diagnosis exceeding eight months.
This is not merely a gap in clinical knowledge-it is a systemic failure of healthcare infrastructure.
Moreover, the increasing prevalence of vestibular disorders in aging populations demands urgent investment in specialized vestibular rehabilitation services, which remain inaccessible to over 58% of rural populations.
Until otoneurology is integrated into primary care curricula and reimbursement structures, patients will continue to suffer avoidable morbidity.
Advocacy, education, and policy reform are not optional-they are imperative.
Aurora Memo
January 12, 2026 AT 10:52I used to think dizziness was just part of getting older
Then I had my first real vertigo episode
It wasn’t anxiety
It was my body screaming for help
And no one listened for months
Thank you for writing this
It’s the first time I felt understood
McCarthy Halverson
January 13, 2026 AT 17:16BPPV is way more common than people think
Try the Epley maneuver before you take another pill
It’s free and works
Jaqueline santos bau
January 14, 2026 AT 16:51Of course they misdiagnose it as anxiety
Women get told they’re hysterical for everything
My sister spent three years on SSRIs because she felt dizzy
Turns out she had vestibular migraine
And now she’s terrified of doctors
How many more women are being gaslit like this
It’s not just medical ignorance
It’s sexism in a white coat
neeraj maor
January 16, 2026 AT 08:24Did you know the FDA approved gentamicin for vertigo because Big Pharma wanted a new profit stream
They’ve been hiding the truth about inner ear crystals for decades
It’s all connected to 5G and the WHO’s global depopulation agenda
They don’t want you to know the Epley maneuver works because it’s too cheap
And VNG tests? They’re just a way to track your brainwaves
They’re using your dizziness to build neural profiles
Next thing you know, your insurance will deny you coverage because your vestibular system is "high risk"
Wake up
Paul Bear
January 16, 2026 AT 17:15While it is commendable that the article elucidates the pathophysiological distinctions between vertigo and dizziness, it is regrettably deficient in addressing the role of cervical vertigo-often overlooked despite robust evidence linking upper cervical spine dysfunction to vestibular symptoms.
Furthermore, the omission of proprioceptive contributions to balance, particularly in patients with degenerative disc disease or chronic poor posture, represents a significant clinical blind spot.
The Epley maneuver, while effective for canalithiasis, does not address cervicogenic vestibular dysfunction, which may present with identical symptoms.
It is therefore misleading to suggest that BPPV is the primary or only mechanical cause of positional vertigo.
Additionally, the assertion that vestibular migraine constitutes 7–10% of cases is statistically inflated; recent meta-analyses suggest a prevalence closer to 3–5%.
Moreover, the claim that "antibiotics are useless for ear infection" is inaccurate when applied to labyrinthitis, which may have bacterial etiology.
While the intent is laudable, the oversimplification of complex neurovestibular pathways undermines the credibility of the entire piece.
Bradford Beardall
January 18, 2026 AT 04:15I’m from India and we don’t have access to VNG machines in most towns
My uncle had vertigo for two years
Doctors gave him motion sickness pills
Finally, his daughter found a YouTube video on the Epley maneuver
Did it at home with a pillow
He was fine in 48 hours
Why do we need fancy tech when simple physics works?
Also, why is this not taught in med school here?
People suffer because no one tells them
chandra tan
January 20, 2026 AT 02:13bro i had this for months
thought i was gonna die
then i did the epley on my bed
felt like a magic trick
why is this not on every doctor’s checklist
Kunal Majumder
January 20, 2026 AT 08:35My mom had PPPD after a bad ear infection
She was told it was stress
Then she found a vestibular therapist
Two months of balance drills
Now she hikes again
It’s not in your head
It’s in your brain’s wiring
And yes, CBT helps
But only if you know what you’re fighting
Ashlee Montgomery
January 21, 2026 AT 14:42What if the real problem isn’t the ear or the brain
But the way we’ve disconnected from our bodies
We sit all day
We stare at screens
We ignore the subtle signals
Then we get dizzy
And we look for a pill
But maybe the body is trying to say: slow down
Not fix the ear
But fix your life
Christine Milne
January 23, 2026 AT 04:04As an American woman who has spent decades fighting for medical equity, I find it deeply troubling that the United States lags behind European nations in vestibular diagnostics.
In Germany, all primary care physicians are required to perform basic positional testing.
In Sweden, vestibular rehab is covered under universal healthcare.
Here, we have billionaires funding space tourism while seniors wait months for a VNG test.
This is not a medical issue.
This is a moral failure.
And until we treat balance disorders with the same urgency as heart attacks, we are complicit in their neglect.
Jake Kelly
January 24, 2026 AT 20:15Just wanted to say thank you
I’ve been dizzy for 18 months
Today I finally asked for a VNG
My doctor didn’t know what it was
But I printed the article
And showed him
He referred me today
Feels like a small win
Ritwik Bose
January 26, 2026 AT 00:09Thank you for this 🙏
I’m from India too
My aunt had vertigo for 4 years
Doctors said "old age"
Then we found a neurotologist in Delhi
She had BPPV
Epley maneuver
Now she dances at weddings again
Knowledge saves lives
Share this